
Heart attack
Did you know that ischaemic heart disease often strikes without warning and remains underdiagnosed, especially in high-risk groups? In Singapore, this silent killer is the third leading cause of death after cancer and pneumonia. According to the latest statistics from the Ministry of Health, it accounted for approximately 5,300 deaths, or 20% of all deaths, in 2023. The number of heart attack cases has also increased by about 44%, from 9,124 cases in 2012 to 13,137 cases in 2022. Among patients who suffered a heart attack, an increasing number – almost 1 in 7 – did not experience any symptoms at all.
WHAT IS IHD?
Coronary artery disease occurs when the arteries that supply blood to the heart muscle become narrowed or blocked due to the buildup of atherosclerotic plaque, which is a mixture of fat, cholesterol and other substances. When this plaque buildup becomes significant enough to impair the flow of oxygen-rich blood to the heart, the condition is termed ischaemic heart disease (IHD).
At this stage, the reduced oxygen supply to the heart muscle – known as ischaemia – tends to be more pronounced during physical exertion, when the heart requires more oxygen. If blood flow to the heart muscle eventually becomes severely reduced by buildup of plaque, or is suddenly blocked when a plaque ruptures and forms a clot, it can damage the heart muscle, leading to a heart attack.
SYMPTOMS OF IHD
The most common symptom is angina – a type of chest pain or discomfort caused by ischaemia of the heart muscle. This discomfort may radiate to the shoulder, arm, back, neck or jaw. It typically occurs with physical exertion, after eating, or during emotional stress, usually lasting a few minutes but rarely more than 30 minutes, and generally resolves with rest or medication.
Alarmingly, for some individuals, the first sign of IHD may be a full-blown heart attack without any prior warning symptoms. A heart attack is characterised by severe, persistent chest pain, often described as a crushing, squeezing or tight sensation lasting continuously for more than 10-15 minutes and not improving with rest. Without prompt treatment, this can lead to irreversible damage to the heart muscle and, in some cases, sudden cardiac death.
Other possible symptoms of IHD include shortness of breath, profuse sweating, nausea or vomiting. In certain populations, particularly older adults, women and individuals with diabetes, symptoms may be atypical and easily mistaken for non-cardiac issues. They may even be completely absent. Atypical presentations include unexplained fatigue or weakness, indigestion like discomfort, back or jaw pain without chest pain, dizziness, or fainting. Such variations in presentation can make accurate diagnosis more challenging and underscore the importance of cardiac health screening, awareness of red- flag symptoms, and timely medical evaluation.
RISK FACTORS FOR IHD
IHD, together with stroke and peripheral vascular disease, encompasses a wide spectrum of conditions termed atherosclerotic cardiovascular disease (ASCVD). Established risk factors for ASCVD can be grouped into modifiable and non-modifiable categories. Non-modifiable risk factors include:
• Age: Risk increases with age, especially in men over 45 and women over 55 years of age.
• Sex: Men are 3-5 times more likely to have IHD than pre-menopausal women, though women’s risk gradually equalises post-menopause.
• Ethnicity: In Singapore, Indians are more likely to have IHD, followed by Malays and then Chinese.
• Family history of premature IHD: Defined as under 55 in male relatives and under 65 years of age in female relatives.
• Genetic factors: These include inherited lipid disorders, such as familial hypercholesterolaemia.

Modifiable Risk Factors
Modifiable risk factors can be addressed through lifestyle changes and/or medical treatment. These include:
• Smoking: One of the strongest modifiable risk factors.
• Hypertension (high blood pressure)
• Hyperlipidaemia (high cholesterol)
• Diabetes mellitus (elevated blood sugar levels)
• Obesity
• Physical inactivity
• Unhealthy diets: Such as those high in saturated fat, trans fats, salt and refined sugars.
• Excessive alcohol consumption: Especially binge drinking or chronic excessive intake
• Psychosocial factors: Including chronic stress, depression and social isolation
In addition, there are emerging risk factors such as lipoprotein(a) (Lp(a)) – a genetically determined particle structurally similar to LDL (“bad cholesterol”) but with an added protein component called apolipoprotein(a). Elevated Lp(a) is an independent risk factor for atherosclerotic cardiovascular disease, including IHD, stroke and aortic stenosis.
WHAT YOU SHOULD DO
If you are concerned that you may be experiencing symptoms of IHD, do not ignore these symptoms. They are your body’s way of signalling something is wrong. Seek medical attention promptly. Depending on the urgency and severity of symptoms, seek immediate care at the nearest emergency department, or schedule an early appointment with a cardiologist.
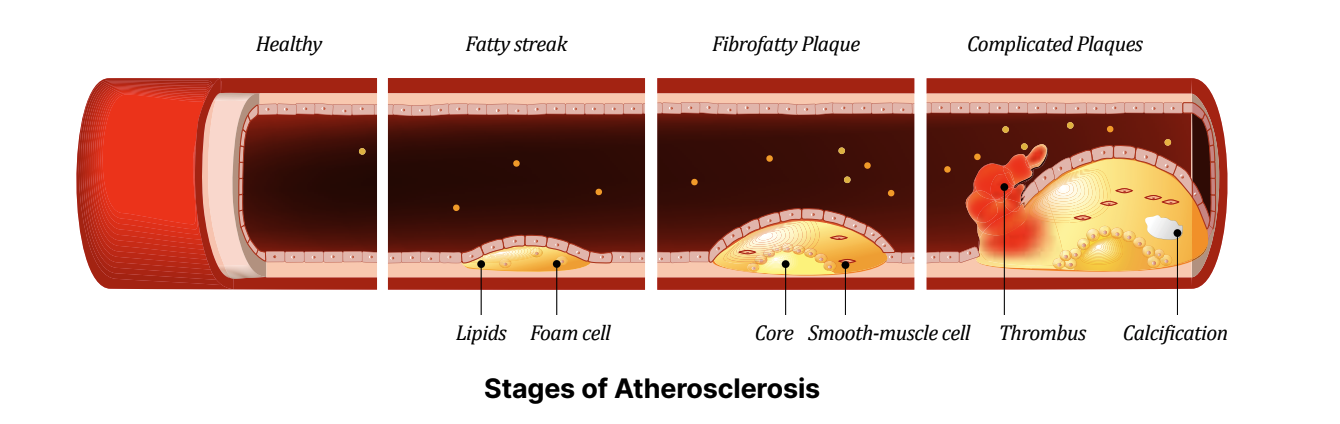
Stages of Atherosclerosis Dr Benji Lim
DIAGNOSIS OF IHD
For diagnosis, a cardiologist will review your symptoms and assess your cardiovascular risk profile. Depending on your condition, your doctor may recommend further investigations, such as blood tests, an electrocardiogram (ECG – a recording of the heart’s electrical activity), a treadmill exercise test, an echocardiogram (ultrasound scan of the heart that assesses its pumping function and condition of its valves), or a CT scan of the heart’s coronary arteries. While these non-invasive methods can detect IHD, they each have their own limitations and may occasionally yield false positives or negatives. In some clinical scenarios, or if non-invasive tests show significant blockages, an invasive coronary angiogram may be required.
CORONARY ANGIOGRAM
A coronary angiogram is a minimally invasive procedure performed under local anaesthesia through a small incision in the wrist or groin. A thin, flexible tube (catheter) is passed through the artery and guided to the heart, where contrast dye is injected into the coronary arteries. A series of X-ray images are taken as the contrast flows through the arteries, revealing any blockages. A diagnostic coronary angiogram typically takes less than 30 minutes to complete. Based on the results of the diagnostic coronary angiogram, there are three main treatment options. Depending on the severity and location of the blockages, treatment can include:
Conservative management:
For minor blockages or blockages in small arteries, medications such as blood thinners and cholesterol-lowering drugs may be sufficient.
Percutaneous coronary intervention (PCI): For severe blockages that are suitable, PCI may be recommended. This involves passing a thin guidewire through the blockage, delivering a balloon along the guidewire, inflating the balloon to open the blockage (angioplasty), and often subsequently placing a stent to keep it open. PCI usually takes 30-120 minutes, depending on complexity.
Coronary artery bypass grafting (CABG): Recommended for complex or multiple blockages (especially in diabetics). CABG is a surgical operation in which a healthy blood vessel (usually from the chest, leg or arm) is grafted to a coronary artery beyond the segment of severe blockage to restore blood flow to ischaemic heart muscles, thereby bypassing the blockage.
In some cases, or when intermediate blockages are detected, further evaluation with coronary physiology tests (e.g. pressure wire assessment) or intra-coronary imaging may help to determine the best course of action.
PCI – Balloon Angioplasty and Stenting
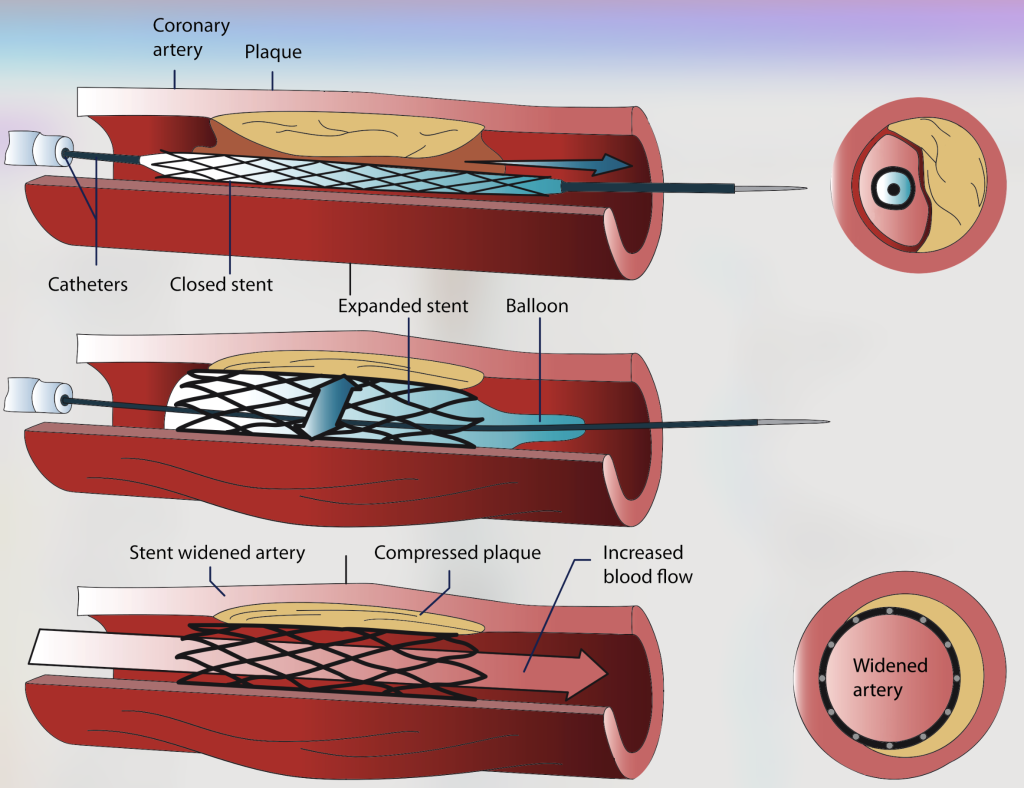
Angioplasty steps
POSSIBLE RECURRENCE
You may think, “If I had a severe blockage that was treated with angioplasty and stenting, I have nothing to worry about now, right?” Well, not quite. While angioplasty and stenting can significantly relieve symptoms and improve quality of life, recurrence is possible if risk factors are not controlled. Recurrence may involve re-narrowing of previously treated areas, or progression of previously minor blockages. Strict adherence to prescribed medications is critical. These medications often include blood thinners (e.g. aspirin, clopidogrel, ticagrelor) and cholesterol-lowering drugs (e.g. statins). Blood thinners reduce the risk of clot formation around stents and the treated segment of the artery – these, if they occur, can lead to a life-threatening heart attack.
Statins have also been proven to reduce cardiac risk by lowering LDL and stabilising cholesterol plaques in the arteries. Lifestyle modifications are equally essential: eat a heart-healthy diet, exercise regularly, quit smoking, and manage conditions such as hypertension, hyperlipidaemia and diabetes aggressively.
CONCLUSION
IHD remains a leading cause of death and disability in Singapore and globally. Fortunately, it is also one of the most preventable. With regular cardiac health screenings, early detection, lifestyle changes and timely medical interventions, individuals can significantly lower their risk. Through increased awareness and proactive care, many can continue to lead active, healthy and fulfilling lives. If you have risk factors or symptoms, speak to your doctor today about a heart health check. PRIME











Leave A Comment