Inflation Solution
Angioplasty means to re-fashion the artery, and in this context, it is used to indicate treatment to a diseased vessel. Angioplasty is commonly used to treat narrowings or occlusions within an artery that reduce blood flow to the part of the body or organ that the artery supplies. Reduction of blood flow to an organ or limb can lead to problems such as organ failure, pain or a reduced ability to fight infection. It may even lead to death.
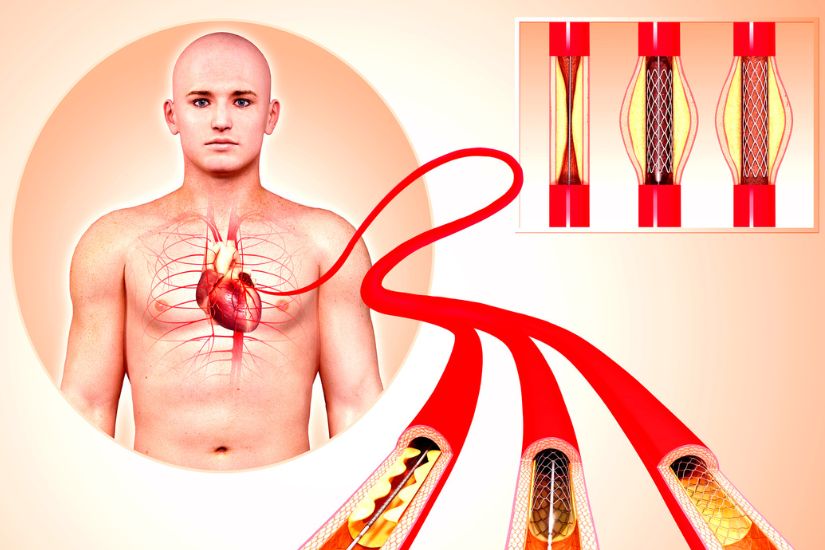
Angioplasty is recommended when blood flow reduction is deemed critical and if left untreated, life or limb threatening problems may arise. In contemporary settings, angioplasty refers to the treatment where a catheter-mounted inflatable balloon is inserted and advanced to the area of narrowing. The balloon is then inflated to “stretch” the narrowing to its original diameter, thereby restoring blood flow after the balloon catheter is removed.
Benefits
The major advantage of angioplasty procedures is its minimally invasive nature. It can effect restorative changes to the diseased artery just like open vascular surgery, but without the need for large incisions. Without large incisions, patients experience less pain, have less risk of wound/incision complications, and also need less recovery “down-time”.
Risks
As with any vascular surgery, the risks of angioplasty include bleeding, bruising, inadvertent clot formation within the artery due to instrumentation, and recurrence of the narrowing/occlusion leading to early failure of therapy. Angioplasty is a form of endovascular surgery where the treatment is rendered from within the artery through a needle stick puncture. To guide treatment, live X-ray (fluoroscopy) and contrast are required to visualize the disease and adequacy of angioplasty. Excessive contrast use can be harmful to the kidneys (contrast nephropathy) but this is uncommon. Patients usually recover fully.
Types of Angioplasty
The commonest form of angioplasty is balloon angioplasty (also known as POBA). Drug-coated balloons (DCB) can be used to deliver medications to the narrowed areas to prolong patency via the same angioplasty technique. Another form of treatment is atherectomy, which is an endovascular technique to debulk the plaque causing narrowing, followed by balloon angioplasty and stenting.
Angioplasty can be used to treat disease in various parts of the body including the carotids (neck arteries for stroke reduction), coronary (heart arteries for treatment of coronary artery disease that can cause chest pain or heart attacks), mesenteric (intestinal arteries that cause lack of blood flow and pain after eating), renal (narrowed kidney arteries that cause high blood pressure), lower extremity arteries (that cause pain/claudication, infection or gangrene), and haemodialysis accesses such as arteriovenous fistulae or grafts in the arm.
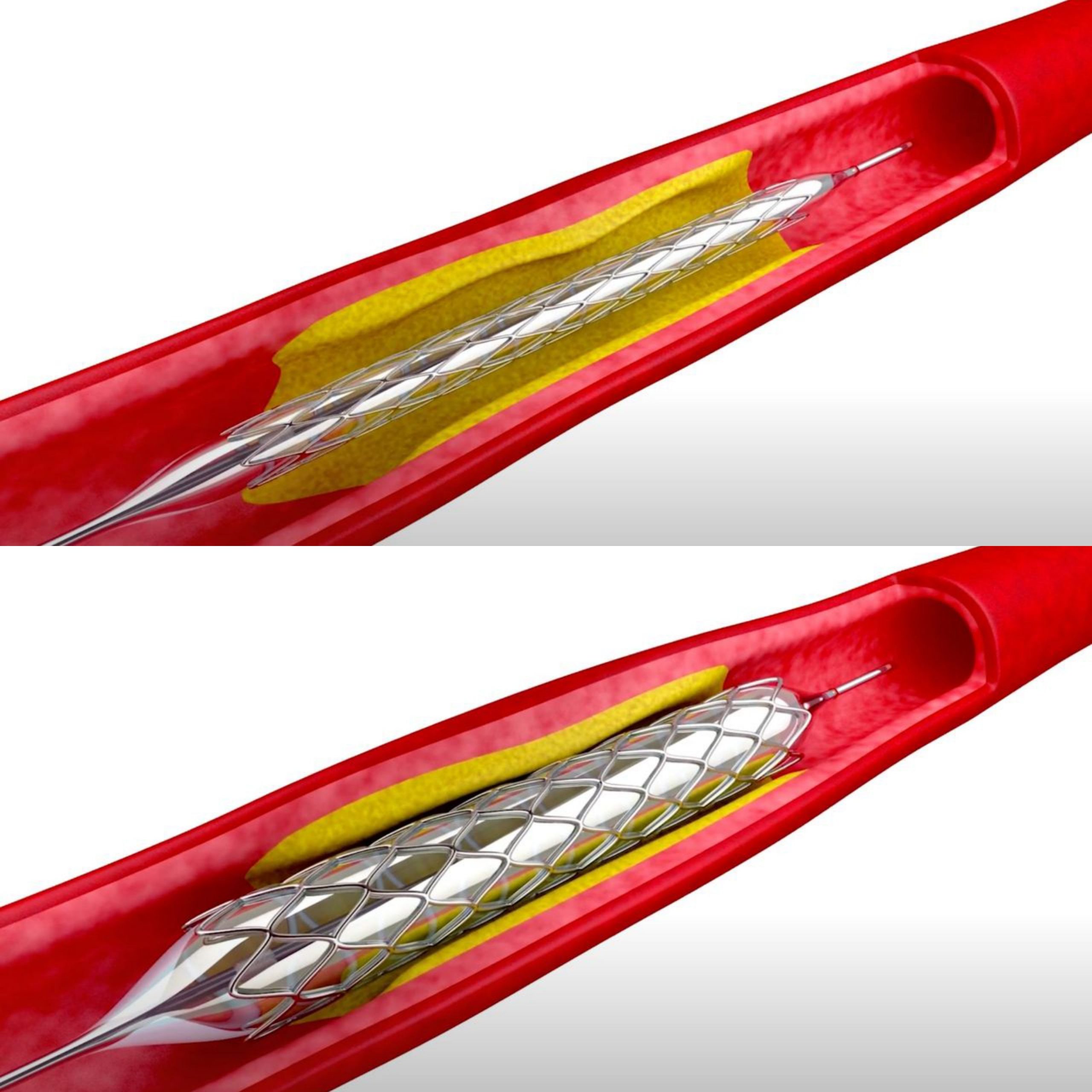
Stents
Stents are scaffold devices that can be implanted inside a blood vessel to keep the narrowing or occlusion from closing back up on itself. The simplest stents are open-cell stents, where a wire mesh is rolled into a tube configuration, crimped to reduce its cross-sectional profile so that it can be passed inside the artery via a needle stick. It is then delivered to the site of narrowing to help the vessel re-expand to its original diameter (effacement). The wire scaffold can be made from different metals or alloys, and have different properties: some have more flexibility while others have more radial strength.
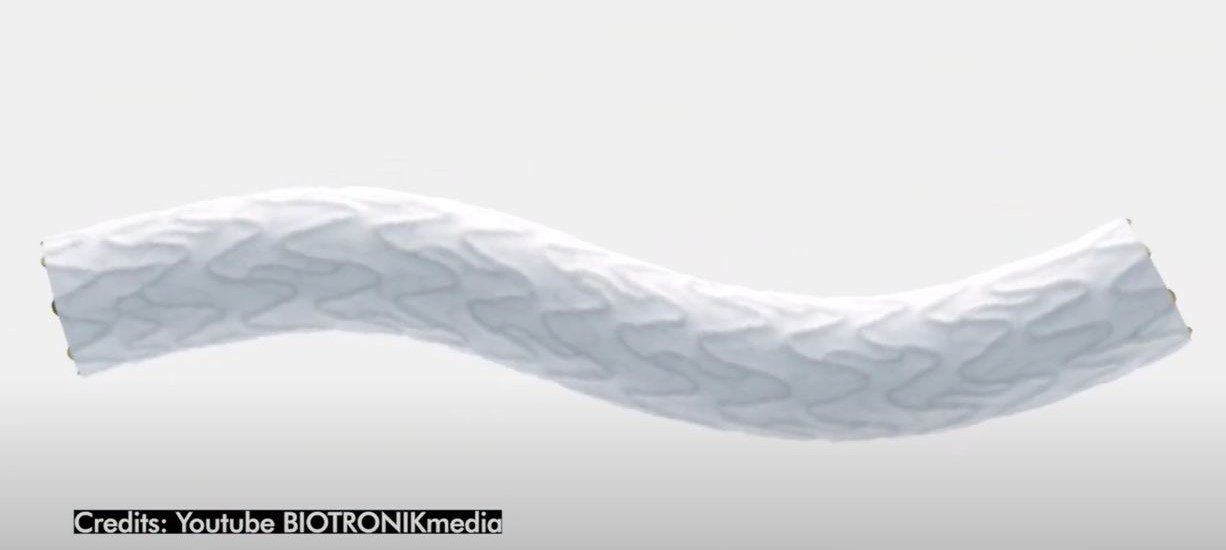
There are also stents which are impregnated with medications that slow-down or prevent recurrence of narrowings or occlusions (drug eluting stents/DES). Covered-stents have an additional thin layer of waterproof material coating that allows blood to flow only within the stent, and are useful in treating bleeding where part of the artery is disrupted. Large diameter covered-stents are used to treat larger arteries such as the aorta, and disease conditions such as aneurysms. They are commonly known as endografts.
Usually, stents are required if angioplasty therapy alone is not adequate. A common example is when an artery narrowing does not stay open despite repeated angioplasty. This is usually the case if the narrowing is due to a hard calcific plaque or a dense fibrotic scar (intimal hyperplasia). Other vascular conditions such as bleeding or aneurysms will require covered-stents to stop the bleeding or exclude the risk of rupture.
Preparation
Patients are best prepared by receiving counselling from a vascular specialist on the indication, method, risks and benefits of the procedure as well as post-procedure expectations. Patients who require additional anaesthesia for the procedure (sedation or general anaesthesia) will need to fast overnight (8-12 hours).
Procedure
Angioplasty procedures are performed under sterile conditions with sophisticated X-ray equipment for imaging. Common venues include a hybrid operating room with full operating room capability and the most sophisticated imaging, cardiovascular angiography suite/laboratory (CVL), or a regular operating room with mobile X-ray imaging equipment. All procedures are performed with anaesthesia for the patient’s comfort, and can vary from just local anaesthesia to intravenous sedation to general anaesthesia. The procedure is minimally invasive and is performed entirely through a needle stick.

Recovery
Depending on the nature of the treatment, angioplasty procedures can be done as an outpatient procedure, day surgery or require a few days hospital stay. For example, angioplasty for haemodialysis access (arteriovenous fistula or grafts) are typically outpatient or day surgery (patient goes home on the same day) procedures, while leg angioplasty for peripheral artery disease can be an overnight stay as long as there are no other medical needs. On the other hand, aortic aneurysms endograft procedures can require 1-3 day inpatient hospital stays.
After an angioplasty procedure, most patients can get back to their regular routines on the same day or the next day.
More complicated angioplasty procedures such as leg angioplasty requiring access via the femoral arteries (at the groin) will require complete bed-rest for 2-6 hours after surgery to reduce the risk of access site bleeding. Some patients in this category will also need close monitoring overnight to make sure post-procedure complications do not arise, as they are generally patients with complex medical problems. This will be true also for open vascular surgery.
The long term limitation of angioplasty is its durability, where the disease (narrowing) recurs earlier than for open vascular surgery. However, there are additional treatment options that can improve the durability of angioplasty results. These include DCB and DES. Moreover, recurrent disease can be treated with repeat angioplasty in the future, thus avoiding the need for open surgery once again.
Post-Angioplasty Follow-Up
Routine follow-up with the doctor is required – initially at short intervals (1-2 weeks) and eventually at 3-6 monthly – to monitor that everything is flowing well. Periodically, an imaging test, such as an ultrasound scan or a CT scan, is required for assessment, depending on the nature of the treatment. Patients will be educated and trained to recognize tell-tale signs that everything is going well (good blood flow) or if there is a problem (flow is reduced again).
In terms of the signs and symptoms that a patient should be aware of post-angioplasty, they include bleeding from the access site, bruising at the treated site and swelling (hematoma). Pain can be associated with cessation of blood flow if the treated segment re-occludes either from the disease or clots that have inadvertently formed. For this reason, many patients are started on blood thinner medications after angioplasty to prevent clot formation. Blood thinner medications come in varying types and potency, and can cause other bleeding problems (nose bleeds).
Dr John Wang
Vascular and Endovascular Surgeon, PanAsia Surgery Group











