Gastrointestinal Cancer Prevention: Guarding Your Gut
Effective Strategies to Protect Your Digestive Health
Gastrointestinal (GI) tract cancers include malignancies that affect the oesophagus, stomach, small intestine, colon, and rectum.
Gastrointestinal cancer prevention is crucial, as these cancers are among the most common and deadly worldwide. Fortunately, simple lifestyle and dietary measures can significantly reduce the risk.
This article explores key GI cancer prevention strategies you can adopt to protect your gut health and lower your chances of developing digestive cancers.

Diet and Gastrointestinal Cancer Prevention
Your diet plays a central role in gastrointestinal cancer prevention. Here are essential ways to support a healthy digestive system:
1. Eat a Healthy, Balanced Diet
Include plenty of fresh fruits, vegetables, whole grains, and legumes. These foods are high in fibre, which helps maintain good digestion and may lower the risk of colon cancer.
Berries, leafy greens, and colourful vegetables are also rich in antioxidants that protect cells from damage caused by free radicals.
2. Limit Red and Processed Meats
Reduce red meats (beef, lamb, pork) and processed meats (bacon, sausages, deli meats). High consumption of these is linked to a greater risk of colorectal cancer.
3. Choose Healthy Fats
Opt for avocados, nuts, seeds, and olive oil instead of saturated and trans fats. This supports weight management and helps lower the risk of obesity-related cancers, including colorectal and pancreatic cancers.
4. Avoid Excessive Salt, Pickled, and Fermented Foods
These have been associated with a higher risk of stomach cancer.

5. Stay Hydrated
Adequate hydration supports a healthy digestive system and may help reduce the risk of certain GI tract cancers.
Lifestyle Habits That Support Gastrointestinal Cancer Prevention
Besides eating well, your daily habits also affect your gut health and overall cancer risk.

1. Limit Alcohol and Tobacco
Excessive alcohol consumption increases the risk of several GI tract cancers, including those of the oesophagus, stomach, and liver.
It is best to drink moderately or avoid alcohol altogether.
Tobacco use is also a major risk factor for GI tract cancers. In addition, certain cooking methods such as grilling, smoking, or barbecuing meats can produce carcinogenic compounds — so limit consumption of such foods where possible.
2. Stay Active and Maintain a Healthy Weight

Regular physical activity helps you maintain a healthy weight and lowers the risk of GI tract cancers.
Studies show that consistent exercise provides protective benefits against various cancers.
Aim for at least 150 minutes of moderate or 75 minutes of vigorous exercise each week.
Obesity and excess abdominal fat are linked to higher cancer risk, so staying active and eating well are essential preventive measures.
3. Manage Stress

While some stress is normal, chronic or severe stress can negatively affect overall health and may influence cancer development.
Stress alone does not cause cancer, but it may interact with other risk factors. Researchers believe that prolonged stress can weaken the immune system, increase inflammation, and trigger cellular changes.
To minimise its impact, practise healthy coping mechanisms such as regular exercise, mindfulness, adequate sleep, and social support.


4. Vaccinations
Some GI tract cancers, such as liver cancer, can result from viral infections like hepatitis B.
In endemic regions like Southeast Asia, hepatitis B vaccination helps prevent liver cancer in high-risk individuals.
5. Minimise Exposure to Carcinogens
Avoid unnecessary exposure to known carcinogens such as pesticides, industrial chemicals, and environmental toxins.
Taking precautions can help lower your risk.
Screening and Early Detection for Gastrointestinal Cancer Prevention
Screening and early detection are vital, as they can lead to better treatment outcomes and improved survival rates.
Common Screening Methods
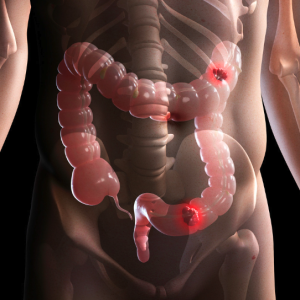
Colonoscopy – The gold standard for detecting colorectal cancer.
It uses a flexible tube with a camera to identify and remove polyps or abnormal growths before they turn cancerous.
Faecal Occult Blood Test (FOBT) or Faecal Immunochemical Test (FIT) –
These non-invasive tests detect hidden blood in stool, which may indicate colorectal cancer.
They should be done annually for accuracy. If positive, a colonoscopy is recommended to identify the source of bleeding.
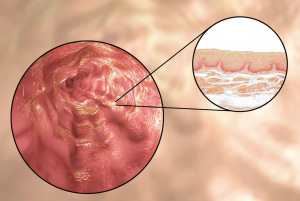
Endoscopy (OGD) – Examines the oesophagus, stomach, and duodenum for abnormalities or early signs of cancer.
Imaging Tests (CT, MRI, Ultrasound) – Used to visualise the GI tract and nearby organs, aiding in diagnosis and staging.
Biomarker Testing (GASTROClear) –
The world’s first approved molecular blood test for early gastric cancer detection.
It classifies individuals as low, medium, or high risk, guiding further investigation when necessary.
Tumour Markers and GI Cancer Monitoring
Tumour markers are substances found in the blood or tissues of some cancer patients. They are produced by cancer cells or by the body in response to cancer.
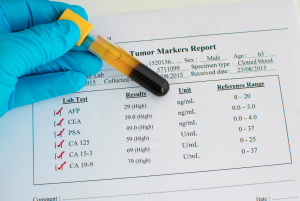
These markers can help with cancer screening, monitoring treatment response, or detecting recurrence.
However, they are not reliable as standalone tools for GI tract cancer screening due to:
-
Limited Specificity: Levels may rise in non-cancerous conditions, leading to false positives.
-
Low Sensitivity: Early-stage cancers may not elevate marker levels enough for detection.
-
Varied Expression: Not all GI cancers produce detectable tumour markers.
Therefore, tumour markers should be viewed as supportive, not diagnostic, tools — best used alongside imaging and endoscopy.
Choosing the Right Screening Method
Before screening, ask yourself:
“Do I have any symptoms, especially those related to the digestive tract?”
If yes, consult your doctor for a detailed assessment. You would not be considered part of the asymptomatic screening population.
If no, and you feel well, consider the following:

1. Colorectal Cancer Screening
If you have a family history of colorectal cancer in a first-degree relative (parent or sibling) diagnosed before age 50, a colonoscopy is recommended.
It detects pre-cancerous lesions early.
If you have no family history, you are at average risk.
For those aged 50 and above, FIT testing once every two years is advised. Annual testing increases sensitivity.
Alternatively, the Ministry of Health now allows Medisave claims for screening colonoscopy once every 10 years.
2. Gastric Cancer Screening
Helicobacter pylori infection increases stomach cancer risk.
You can test for it using a blood test (for antibodies) or a urea breath test (for active infection).
Testing is advisable if your spouse or parents have had this infection.
Another option is the GASTROClear blood test, which can guide whether further endoscopic evaluation is needed.
3. Oesophageal Cancer
Currently, there is no effective screening test.
If you experience frequent or severe heartburn or acid reflux, consult your doctor about endoscopic evaluation.
4. Liver Cancer (Hepatocellular Carcinoma)
Chronic hepatitis B infection is a key risk factor.
If you are a hepatitis B carrier, regular blood tests and ultrasound scans are essential for early detection and treatment.
Conclusion
Screening plays a crucial role in detecting GI tract cancers early and improving survival outcomes.
However, prevention goes beyond screening.
A balanced diet, regular exercise, maintaining a healthy weight, and avoiding tobacco and excessive alcohol are equally important.
Combining these strategies with timely screening can significantly reduce the risk and burden of GI tract cancers. PRIME











Leave A Comment