Rear Agony
Piles: Protector or a Pain? Time to Debunk the Myths!
Haemorrhoids, commonly known as piles, are a very common condition in Singapore, with up to one in three people suffering from this condition. Most people get embarrassed and do not consult their doctor about the condition until there is significant bleeding, pain and/or prolapse, which affects their quality of life.
In fact, haemorrhoids are normal and present in everyone. They are located in the mid anal canal and are often known as anal cushions comprising blood vessels, which serve a specific purpose of preserving continence.
In this article, I will talk about some of the most common myths surrounding piles and help everyone gain a better understanding of the condition.
Myth 1: Haemorrhoids or piles are abnormal, and should always be removed.
FALSE!
Haemorrhoids (or piles) are a normal part of our body, specifically the anus. Together with the anal muscles, they are part of our important continence mechanism – they help us to hold in our stools. As such, they should be left alone if they are not causing problems.

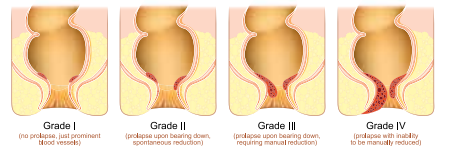
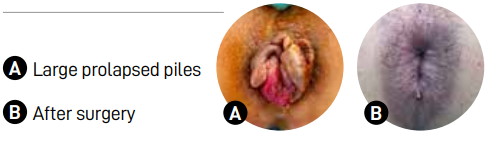
Treatment is only necessary when piles become problematic and develop symptoms. This is known as haemorrhoidal disease. Most commonly, patients will present with bleeding (usually fresh and bright red), pain and prolapse (large protruding piles), or a combination of these three complaints.
Myth 2: Haemorrhoids only affect the elderly.
FALSE!
Piles can affect any age group, but the most common age group affected is between 20-40 years old. In my practice, this group comprises about 75% of my patients. However, the risk does increase with age, and ladies are more likely to be affected, especially after childbirth.
Myth 3: If I am young, healthy and doing sports regularly, I should not be affected by piles, especially since I’m eating lots of fibre!
FALSE!
I have seen an uptick in the number of cases in recent years. I estimate that there has been a 20% year-on-year increase in the number of patients who had seen me for this problem in the past 5 years. The contributing factors are primarily lifestyle related, comprising dietary habits, toileting habits, and the performance of certain sports/exercises.
A multitude of dietary fads, ranging from keto diet to veganism, has led to abnormal alterations in our bowel patterns as well as, more importantly, our stool consistency. The lack of a balanced diet (i.e., everything should be eaten in moderation, including fibrous foods like vegetables, fruits, whole grains, bran, oats, etc.) can lead to problems at both ends of the dieting spectrum. In fact, the vast majority (80%) of my patients develop constipation are eating too much fibre! They all have the three cardinal signs of bloating, flatulence and pellet-like/bulky stools (Bristol stool chart type 1 to 2).
Combining the effects of excessive and prolonged straining; sitting on the toilet bowl for too long (gadgets like our handphones and tablets bear the blame here); and the performance of certain sports like weightlifting, it is little wonder that I am seeing more patients suffer from haemorrhoidal disease, especially among the young.
Myth 4: I can decrease the risk of haemorrhoidal disease by exercising more intensely and taking more fibre, so that I can clear my poop daily!
FALSE!
Any exercise that is repetitive and prolonged, especially those involving significant straining such as weights-associated or squatting type exercises, can cause our haemorrhoidal tissue to swell excessively. However, this is usually in relation to other lifestyle factors, such as an unbalanced diet (too much fibre or meat) and spending too much time on the toilet bowl. Together, these factors can cause sustained damage to our piles.
In fact, the common obsession and myth about needing to poop daily have led many people to sit and wait on the toilet bowl unnecessarily, spending a long time on excessive straining. When one sits on the bowl, one’s haemorrhoids will automatically start to swell. However, it should be noted that this is reversible and not detrimental as long as one keeps the time spent on the toilet bowl to between 5-10 minutes.
Myth 5: Piles always needs surgery!
FALSE!
The key is to seek treatment early and identify the triggering factors in your lifestyle, such as your diet, your toileting habits and your exercise routine. These actions, together with understanding and debunking the myths surrounding piles, are vital for the effective and long-term relief of symptoms. There are three key steps you need to take.
Step 1: Correct the underlying triggers, such as improper dietary and toileting habits.
Step 2: Start medications. This may include a combination of tablets, suppositories and creams.
Step 3: In cases where steps 1 and 2 fail or in severe cases, surgery can be helpful. In terms of surgery, I would advise merely removing the excessive/swollen parts and leaving the normal haemorrhoidal tissue intact. This is so that the patient can remain continent for stool voiding.
More importantly, I always emphasise to my patients that unless they correct their lifestyle triggers, the problem will recur as piles are still present in the anus to perform its function. The treatment of piles requires a team effort. It is about understanding and debunking dietary and toileting myths.
Myth 6: Bleeding from the bottom is always due to piles!
FALSE!
While bleeding from piles is very common, the causes vary, and they may signal a more deadly condition like colorectal cancer (CRC). This is particularly worrying in Singapore, where CRC is the most common cancer in the country (1st in men and 2nd in women). You must never assume that your bleeding is due to piles and ignore the problem.

What is even more alarming is that we are seeing more young CRC patients, with up to one in five CRC patients diagnosed being below the age of 50 years. Hence, if your bleeding is coupled with other symptoms like looking pale, feeling tired and weak, and unexplained loss of weight or appetite, you should seek medical attention early to exclude CRC.
My recommendation is to have a colonoscopy done from the age of 45 (if you are well with no symptoms); or earlier if you exhibit the aforementioned symptoms or 10 years before the age of the first CRC case in your family, whichever takes place earlier.
The good news is that if a pre-cancerous polyp is removed during colonoscopy, CRC can be prevented. If an early cancer is detected and treatment starts promptly, the results are often very good. However, at these early stages, it should be noted that most patients do not display the classic symptoms of pain, bleeding and weight loss. The latter is a symptom that often signals late advanced cancer.
So come early for your colonoscopy as it could save your life!
Myth 7: Probiotics are not useful for piles problems.
FALSE!
As mentioned earlier, the treatment of piles involves identifying the triggers, optimising lifestyle behaviours (including dietary and toileting habits), and taking medications, with surgery being the final resort.
Having said that, probiotics are still a very useful adjunct to treating and preventing piles problems. They help to regulate stool consistency, and maintain type 4 stools (i.e., banana or sausage shaped stools). Type 4 stools are ideal and the least traumatic to piles tissue as they pass through the anal canal more easily.
Taking probiotics regularly also helps to improve gut health and overall immunity. This, in turn, reduces the risk of diarrhoea (from infections), which causes piles to swell, leading to symptoms.

Dr Mark Wong Te Ching
Senior Consultant
General & Colorectal Surgeon
Mark Wong Surgery
Dr Mark Wong is an Adjunct Asst Professor and Senior Consultant Colorectal & General Surgeon practising at Mount Elizabeth Novena and Mount Alvernia Hospitals. After graduating in 1999 from NUS, he was awarded a Gold Medal for his Surgical Fellowship from Edinburgh in 2008 and was appointed Adjunct Assistant Professor at the Duke-NUS Graduate Medical School. He then completed a prestigious double MOH fellowship in minimally-invasive (robotic and laparoscopic) colorectal cancer and pelvic floor surgery in France (2010) and Denmark (2014). Dr Wong is an opinion-leader and is widely published in these fields of surgery. Prior to leaving for private practice, he practised at SGH, where he was Director of the SGH Pelvic Floor Disorders Service and Gastrointestinal Function Unit.

Mark Wong Surgery
Mount Elizabeth Novena Specialist Centre
38 Irrawaddy Rd #08-31
Singapore 329563
Tel: +65 6261 4883
Mount Alvernia Hospital Medical Centre A
820 Thomson Road #02-03
Singapore 574623
Tel: +65 6356 4088
WA: +65 9125 8390
Website: www.markwongsurgery.com
FB: www.facebook.com/markwongsurgery
IG: www.instagram.com/markwongsurgery
LI: www.linkedin.com/company/mark-wong-surgery
TT: www.tiktok.com/@drmarkwong











