Developments and things to note in the fight against diabetes

During the 2017 National Day Rally, Prime Minister Lee Hsien Loong painted a stark picture of the diabetes situation in Singapore as he encouraged citizens to exercise more, go for regular medical check- ups and eat healthier. He cited sobering figures: One in nine Singaporeans has diabetes, while three in 10 over the age of 60 have diabetes. Broken down by race, 2.5 in 10 Chinese over 60 years old have the disease as well as half of Malays over 60 years old and six in 10 Indians over that age. He called the disease “one of three key long-term issues for Singapore” and said, “It is precisely because many people are not worried that I am worried. It is precisely because many people do not take diabetes seriously that it has become a serious problem.”
COMMON CAUSES AND TREATMENTS FOR DIABETES

Most people are aware that there are different types of diabetes and different causes are associated with each type of diabetes. For Type 1 diabetes, an autoimmune disease, doctors remain unsure about the causes. For this type of diabetes, the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. While it is possible that genes may play a role, it is also possible that a virus sets off the immune system attack. About 10% of people with diabetes have this type. Type 2 diabetes stems from a combination of genetics and lifestyle factors. Obesity increases the risk of type 2 diabetes. Carrying extra weight makes cells more resistant to the effects of insulin on blood sugar. This condition runs in families as members share genes that make them more likely to get type 2 diabetes and to be overweight. There is also gestational diabetes which is the result of hormonal changes during pregnancy.
Doctors treat diabetes with a variety of medication. Insulin is commonly used as the main treatment for type 1 diabetes. It replaces the hormone that the body is unable to produce. In terms of type 2 diabetes, diet and exercise are used to help people manage the disease. Further to this, a variety of drugs to lower blood sugar levels may also be used if lifestyle changes are not enough to manage the disease.
Beyond the use of insulin and other drugs as well as the implementation of lifestyle changes, there have been other medical developments that can help to control and manage this illness in the future.
SMART INSULIN

One of these developments is the creation of a “smart” insulin that could reduce dangerous complications in people who use the drug to manage diabetes. This new type of insulin, called i-insulin, is released for action when the blood sugar or glucose levels rise and blocks its own activity when glucose levels fall. What happens is that at low glucose levels, the i-insulin is bound to the glucose transporter and is inactive. When glucose levels rise, such as after a meal, the higher glucose competes with the i-insulin for glucose transporter sites and as a result, insulin is released into the blood stream to dock with its lock and lower glucose levels.
Further pre-clinical tests and subsequent clinical trials in humans will be required before the smart insulin will be made available to patients. However, the vision, if realised, would be one of the most exciting advances in diabetes care.
PANCREATIC ISLET TRANSPLANTATION
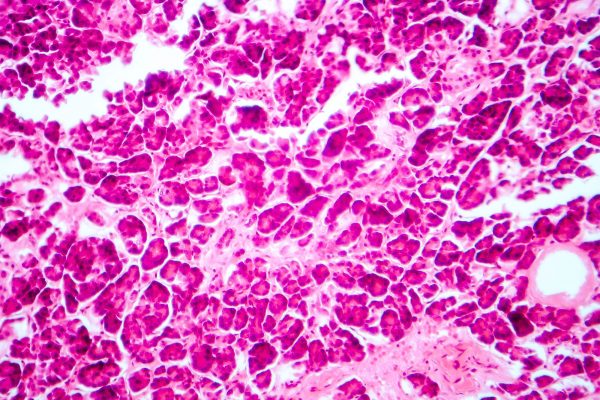
Pancreatic islet transplantation is an experimental treatment that is currently under clinical trial in the US for type 1 diabetes. The process involves doctors taking islets with healthy beta cells from the pancreas of an organ donor. The healthy islet cells are then injected into a vein that carries blood to the liver of a recipient. These islets begin to make and release insulin in the recipient’s body. More than one injection of transplanted islet cells is often needed to stop using insulin.
Not all people with type 1 diabetes are good candidates for islet transplantation. Certain people with type 1 diabetes who have blood glucose levels that are difficult to manage, experience severe hypoglycemia and have hypoglycemia unawareness, a dangerous condition in which a person cannot feel or recognise the symptoms of hypoglycemia, may be candidates.

People who have type 1 diabetes and have had, or are planning to have, a kidney transplant to treat kidney failure may also be candidates. Doctors consider people for islet transplantation if the possible benefits, such as being better able to reach blood glucose targets without problems such as hypoglycemia, outweigh the risks, which includes the possible side effects of immune-suppressants. Immuno-suppressants are medication that recipients must take to prevent their immune system from attacking and destroying the transplanted islets. Kidney transplant patients already take immuno-suppressants and therefore, the risk of islet transplantation is not higher for them.
The possible benefits of pancreatic islet transplantation include improved blood glucose levels, lesser or no need for insulin injections to manage diabetes, fewer or no episodes of severe hypoglycemia and improved awareness of hypoglycemia, which helps prevent episodes of severe hypoglycemia.
Doctors treat diabetes with a variety of medication. Insulin is commonly used as the main treatment for type 1 diabetes. It replaces the hormone that the body is unable to produce.
ACTIONABLES

Beyond the innovative products and procedures that can help to ease the burden of diabetic patients in the future, dealing with present everyday struggles of diabetes is a harsh reality. We need to continue doing the best that we can to combat this disease. This includes:
• Urging people you know who are older than 45 or at risk of diabetes to get a diagnostic blood test;
• Talking to your doctor about your results and what it might mean for your diabetes management and/or blood glucose control;
• Eating healthy carbohydrates, such as fruit, vegetables, and whole grains. This is essential for living well with diabetes as it provides important vitamins and minerals that your body needs;
• If diagnosed with diabetes, strive for excellent control of blood glucose, blood pressure, and blood lipids early on. If you have had diabetes for years and less-than- tight control, it is never too late to improve now;
• Cut down on processed foods, restaurant foods, and using the saltshaker. Blunt sodium’s effects on your blood pressure;
• Lose some weight (5-10kg) early in the course of type 2 diabetes. Keeping it off can improve blood glucose control and prevent or delay heart disease; and
• Take a very active role in managing your diabetes

Get a copy of our latest PRIME magazine










