Understanding the Immune System and Latent Infections
A healthy immune system protects the body and keeps dormant infections under control. A latent infection is one that remains in the body without causing symptoms because the immune system prevents the infection from damaging tissues.
In Asia, hepatitis B is a common infection that can persist after the initial illness. It often becomes latent, staying hidden but capable of reactivating if the immune system weakens.
Understanding Hepatitis B
Hepatitis B virus (HBV) infection is a global health issue. The World Health Organization (WHO) estimates that about two billion people have been infected at some point, and roughly 257 million live with chronic HBV infection. In 2015, approximately 887,000 people died from HBV-related liver disease. Southeast Asia ranks among the top three regions worldwide for chronic HBV infection.
How HBV Persists in the Liver
HBV targets liver cells. During infection, the virus’s partially double-stranded DNA (rcDNA) enters the cell nucleus, where it repairs itself into a stable form known as covalently closed circular DNA (cccDNA).
Even after a patient recovers clinically, small amounts of cccDNA remain in liver cells. This explains why hepatitis B can reactivate later, especially when the immune system is suppressed.
How Hepatitis B Spreads
HBV spreads when body fluids or blood from an infected person enter the bloodstream of someone who isn’t immune. Transmission may occur through:
-
Contaminated blood transfusions
-
Sharing unsterilised or reused needles, including for tattoos or acupuncture
-
Unprotected sexual contact
-
From parent to child during birth
Always ensure that medical, tattooing, or acupuncture needles are new or properly sterilised before use.
Recognising the Symptoms
HBV infection can appear suddenly (acute), flare up after a period of inactivity (reactivation), or be discovered incidentally during a blood test.
Symptoms range from mild fatigue and nausea to severe liver inflammation and failure. Many people remain asymptomatic but show abnormal liver function tests.
The likelihood of developing chronic HBV infection depends on age: about 90 % of infants infected at birth become chronic carriers, compared to less than 5 % of adults. Long-term infection can cause cirrhosis and increase the risk of liver cancer.
Diagnosing Hepatitis B
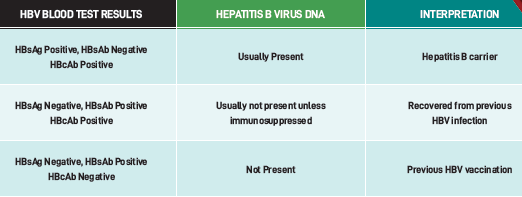
Doctors use several blood tests to assess HBV status:
-
HBsAg (surface antigen) – presence indicates current infection. If positive for more than 6 months, the infection is chronic.
-
Anti-HBs (surface antibody) – indicates immunity from vaccination or past infection.
-
Anti-HBc (core antibody) – indicates prior exposure to HBV.
-
HBV DNA level – measures the amount of virus in the blood. Rising levels may signal a flare or reactivation.
When Steroids Suppress the Immune System
Steroids are affordable and highly effective medications used to treat many inflammatory and autoimmune conditions. They were among the first drugs proven to reduce deaths in severe COVID-19 cases, especially for patients needing oxygen or ventilation.
However, steroids suppress the immune system. Prolonged or high-dose use can trigger HBV reactivation in people with prior infection. Conditions commonly treated with steroids include:
-
Systemic lupus erythematosus (SLE)
-
Inflammatory bowel disease
-
Rheumatoid arthritis
-
Asthma and chronic obstructive pulmonary disease (COPD)
The risk of HBV flare increases with higher steroid doses and longer treatment duration.
Cancer Treatments and HBV Reactivation
Receiving a cancer diagnosis can be overwhelming, and treatment delays due to infection can cause unnecessary anxiety.
Chemotherapy remains a cornerstone of cancer management, given before or after surgery to improve long-term survival or achieve a cure. Many chemotherapy drugs, as well as some targeted therapies and immune checkpoint inhibitors (ICIs), weaken or alter immune responses, which can allow HBV to reactivate.
Certain medications, such as rituximab (a monoclonal antibody targeting CD20), carry a high risk of HBV reactivation. Oncologists work closely with gastroenterologists and hepatologists to ensure patients with a history of hepatitis B can begin and continue treatment safely.
Preventing Reactivation and Managing Treatment
Before starting steroids, chemotherapy, or other immunosuppressive therapies, patients should ask their doctors about HBV screening.
HBV blood tests identify two main risk groups:
-
HBsAg positive / anti-HBc positive: usually have detectable HBV DNA and are at high risk of reactivation.
-
HBsAg negative / anti-HBc positive: generally have undetectable HBV DNA and are at lower risk, but still need monitoring.
Medications for Hepatitis B Control
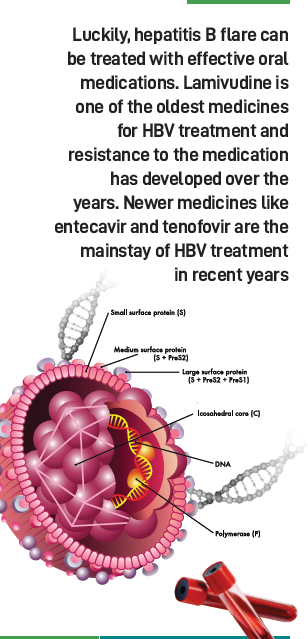
Modern antiviral therapy makes HBV flares preventable and manageable.
-
Lamivudine was one of the first oral antivirals but often leads to resistance.
-
Entecavir and tenofovir (available as TDF and TAF) are now preferred for their potency and low resistance risk.
For people who are pregnant, tenofovir disoproxil fumarate (TDF) has the most established safety record. Tenofovir alafenamide (TAF) is newer, and early evidence suggests similar safety and effectiveness.
Doctors select medication based on risk level, treatment history, and overall health. In high-risk cases, antiviral therapy starts before immunosuppressive treatment and continues for 6–12 months afterward (or longer for high-risk regimens such as rituximab).
Even when HBV DNA becomes undetectable, cccDNA can remain, so careful follow-up is essential.
Coordinated, Patient-Centred Care
HBV management is most effective when guided by a multidisciplinary team. Gastroenterologists, hepatologists, oncologists, and other treating physicians collaborate to ensure safe, uninterrupted care.
When immunosuppression is necessary, early screening and timely antiviral therapy protect patients from complications, allowing treatment to proceed smoothly.
This coordinated approach embodies patient-centred care — tailored, evidence-based, and focused on each individual’s needs.
Call: +65 6322-6333
Whatsapp: +65 9655-2101
email: info@starmedspecialist.com
Website: starmedspecialist.com














Leave A Comment