The liver is a fascinating organ. It is the largest organ in our body, and an adult human liver can weigh approximately 1.5kg. It plays a crucial role in more than 500 vital functions, including the trapping and destroying of bacteria; the detoxification of toxins; the production of bile; the synthesis of proteins, clotting factors and hormones; the regulation of metabolism; and the storage of glycogen, iron and vitamins. Essentially, the liver is the workhorse in our bodies that multitasks. It is a filter, a factory and a warehouse. Considering the many roles it plays, we may very well consider the liver as the king of our internal organs.
LIVER FIBROSIS AND CIRRHOSIS
Our liver is unique in that it repairs and regenerates itself after damage. A liver can potentially regrow to its normal size even after surgical removal of as much as 90% of the native liver. This is a miracle! However, our liver is not invincible. Although a single episode of liver injury may not lead to any long-term consequence upon recovery, repetitive or continuous injury to the liver either through inflammation or accumulation of bile can lead to liver fibrosis.
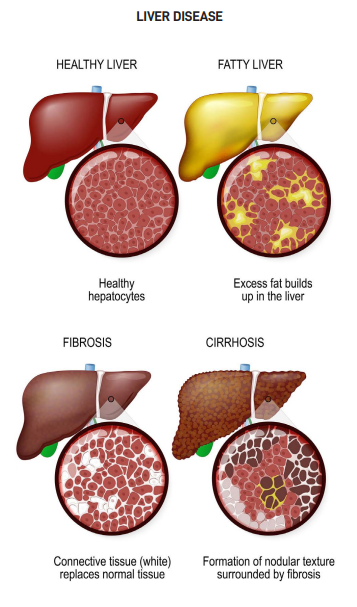
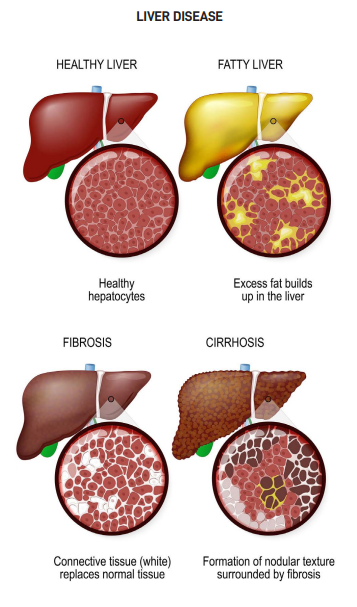
Liver fibrosis is the excessive accumulation of extracellular matrix proteins, including collagen. It is a dynamic process that reflects imbalance in extracellular matrix turnover. This process may be reversed if the underlying cause of liver injury is identified and treated. However, as continuous or repetitive injury usually occurs over a period of months or years, liver fibrosis can become widespread and permanent. It forms bands throughout the liver with distortion of the liver architecture and formation of regenerative nodules. This is called liver cirrhosis. Such liver is often shrunken, and its functions compromised. It is an irreversible manifestation of end stage liver disease. Liver cirrhosis is commonly called scarring or hardening of the liver.
SYMPTOMS
People with early liver cirrhosis often do not have any symptoms as the liver can still function sufficiently to cope with the demands of the body. This stage is called compensated cirrhosis.
As cirrhosis progresses and becomes more advanced, the liver struggles to cope and this leads to decompensated cirrhosis. The following symptoms may then occur:
- Jaundice (Yellow tint in the white of eyes).
- Itchy skin.
- Spider naevi (Spider-like blood vessels surrounding small red spots on the upper chest wall).
- Easy bruising and bleeding.
- Swelling of the feet, ankles and legs.
- Ascites (Distended and fluid filled abdomen).
- Encephalopathy (Sleep disturbance, personality change and confusion).
- Bleeding varices (Vomiting of blood or passage of black tarry digested blood in stool due to rupture of expanded blood vessels in oesophagus).
- Loss of libido, shrunken testicles, enlarged breasts (For men).
- Premature menopause (For women).
- Other non-specific symptoms like lethargy, loss of appetite and loss of weight.

COMPLICATIONS AND PROGNOSIS
Common complications of cirrhosis include ascites, encephalopathy, bleeding varices, infection, kidney failure, liver failure and liver cancer.
When compared with the general population, people with compensated cirrhosis have five times increased risk of death, while people with decompensated cirrhosis have ten times increased risk. Median survival rate of people with compensated cirrhosis is about 12 years, whilst it is two years for those with decompensated cirrhosis.
PREVALENCE
Based on data from a Global Burden of Disease study, it is estimated that 112 million and 10 million people worldwide are living with compensated and decompensated cirrhosis respectively. Liver cirrhosis also attributes to about 1.3 million deaths annually. Locally, the corresponding figures are 122,000 for compensated cirrhosis (age-standardised prevalence rate of 1,919 per 100,000); 13,000 for decompensated cirrhosis (195 per 100,000); and 254 annual deaths (3.7/100,000).
CAUSES
Common causes of cirrhosis include chronic hepatitis B (HBV), chronic hepatitis C (HCV), alcoholic liver disease (ALD) and non-alcoholic fatty liver disease (NAFLD). Other rarer causes include autoimmune liver diseases, such as autoimmune hepatitis, primary biliary cholangitis, and inherited diseases, such as Wilson’s disease and haemochromatosis.
HEPATITIS B (HBV)
HBV is the most common cause of liver cirrhosis and liver related mortality worldwide, contributing to about 30% of cases. The percentage is higher in countries which have a higher prevalence of HBV. Worldwide, there are around 296 million people who are living with HBV. Sadly, only about 10% of these people are aware of their infection. In Singapore, 3.6% of the population aged 18-79 are HBV carriers, and HBV contributes to about 50% of liver cirrhosis as well as liver related mortality.
HBV is transmitted by blood or body fluids, such as semen, from infected persons to people who are not infected. Transmissions commonly occur through childbirth – from mother to child, sexual intercourse, sharing of needles or drug injecting equipment, sharing of razors or toothbrushes, and occupational needle stick injury. While some newly infected HBV people do recover fully, others go on to develop chronic infection which, in due course, may lead to liver cirrhosis and liver cancer. The risk of chronic infection is related to the age at which infection occurs. About 90% of infants with HBV go on to develop chronic infection, whereas for adults, it is only 5%.
The best way to prevent HBV is through vaccination. In Singapore, universal vaccination against HBV was implemented in 1987, so all babies born thereafter would have been vaccinated. People who are not vaccinated should consider getting the vaccination with their general practitioners.
For those with chronic HBV, there are effective medical treatments to suppress the HBV virus and prevent further progression of liver disease.
Some HBV carriers do not require treatment, and only need intermittent monitoring with blood tests and ultrasound scans. In these cases, follow-up is important for early detection of HBV flare as well as the development of liver cancer.
HOLIDAY DRINKING
Mankind has a long history in alcohol consumption. There is evidence to suggest that fermented beverages existed as early as the stone age. Alcohol consumption can be a double-edged sword. For many, alcohol is a must-have for joyous celebrations and important ceremonies; to others, alcohol is a poison that damages their livers and their lives. In Singapore, ALD is the second most common cause of liver cirrhosis and liver related death, accounting for 15% of cases.
Drinking within recommended limits can be safe and enjoyable, but how much is too much? The Singapore Health Promotion Board (HPB) recommends that men consume no more than two standard alcoholic drinks a day, while women should consume no more than one a day. A standard alcoholic drink is defined as a can (330ml) of regular beer, half a glass (100ml) of wine or a nip (30ml) of spirit.
A commonly asked question is whether binge drinking during the festive seasons is safer compared to regular daily drinking. Binge drinking is defined as drinking five standard drinks or more for men and four standard drinks or more for ladies. While daily drinking is the most significant risk factor for ALD, binge drinking may accelerate alcohol-use disorders. It is the most common and deadly pattern of excessive alcohol use in the US. In short, binge drinking and excessive daily drinking are both harmful, and people who drink regularly also tend to indulge in binge drinking.
Studies have shown that 4.3% of male and 0.8% of female Singaporeans drink alcohol regularly, while one in 32 Singaporeans aged 18 and above abuse alcohol. These numbers are trending upwards due to increasing affluence, the easy availability of alcohol as well as greater social acceptance and tolerance towards alcohol drinking, especially among younger Singaporeans.
THE FUTURE
Incidence of liver cirrhosis is predicted to continue to rise in the next few decades. This is likely due to the increasing burden of ALD and NAFLD. Globally, out of the two billion people who drink alcohol, 75 million of them are heavy drinkers and are at risk of developing ALD. On the other hand, there are an estimated two billion adults who are obese or overweight, and about 400 million adults who have diabetes, rendering them at risk of developing NAFLD.
PREVENTION
Prevention is always better than cure. Preventing the occurrence of liver diseases is the most effective way to prevent liver cirrhosis. For healthy people without known liver disease, the following strategies may help to prevent the development of liver diseases:
- Screen for and get vaccinated against HBV.
- Avoid direct contact with other people’s blood or body fluids. This helps to avoid contracting HBV and HCV.
- Drink alcohol in moderation and within the recommendation of HPB (One drink a day for females and two drinks a day for males).
- Maintain a healthy diet and exercise regularly. Maintain a healthy weight and for those who are overweight, aim to lose weight. This helps to avoid NAFLD.
- See your doctor regularly. Go for liver health screening as it helps to detect asymptomatic liver diseases, especially during the early stages. Check for other conditions, such as diabetes, high blood pressure and high cholesterol, that are associated with NAFLD.
- Avoid taking unnecessary medicines or supplements. For those with liver diseases but without cirrhosis, regular medical follow-ups are important for appropriate treatment and advice. These will help to stop further progression of liver disease and hence, prevent the formation of liver cirrhosis.
PARTING ADVICE
Stay motivated and stay active. Adopt a healthy lifestyle and diet. Avoid drinking alcohol altogether and avoid taking unnecessary medication. Also, attend regular medical followups for advice, treatment and surveillance tests.
Contributed by:
Dr. Robert Lo
Senior Consultant in Gastroenterology & Hepatology
Asian Healthcare Specialists (AHS),
Cornerstone Asia Health (CAH)
MB BCh BAO, B Med Sc, MRCP (UK), FEBGH, MD, FRCP (Edin)
https://asianhealthcare.com.sg/












