
Flat feet (pes planus) are common, affecting up to 20-30% of the adult population. While many people live pain-free with flat feet, others develop discomfort or functional problems that require attention.
This article explores situations when flat feet are simply a normal anatomical variation and when to be concerned, and how to manage them from conservative care to modern, minimally invasive surgical options.
1. Flat Feet as a Normal Variant
Many adults have flexible flat feet arches that flatten while standing but reappear when sitting or standing on tiptoe. In most cases, this is harmless and doesn’t require treatment.
✅ Key Points:
- Genetic factors play a role in certain populations having higher rates of flat feet.
- Many children outgrow flat feet as their arches develop naturally by the age of 10.
- Adults with asymptomatic flexible flat feet typically don’t experience future issues.
When to Monitor:
- If there’s no pain, fatigue or functional limitation, flat feet are usually just a normal variation.
- Watch for any signs of discomfort, imbalance or difficulty with prolonged standing or walking.
2. Conservative Treatment: When & How to Intervene
When flat feet become symptomatic, non-surgical treatment is the first step. The goal is to reduce strain, improve alignment and restore function.
A. Custom Orthotics & Supportive Footwear
- Custom insoles help redistribute pressure, correct overpronation, and support the arch.
- Supportive shoes with firm heel counters and arch support add stability and reduce fatigue.
B. Stretching & Strengthening
- Gastrocnemius (calf) stretching improves ankle mobility and reduces strain on the arch.
- Strengthening exercises focus on the tibialis posterior, intrinsic foot muscles and hips to support better foot posture.
- Gait retraining can correct faulty movement patterns that worsen flatfoot symptoms.

📊 A 2020 study in Foot & Ankle International found that a combination of custom orthotics and strengthening reduced pain in 76% of patients with symptomatic flat feet.
Who Benefits Most?
- People with mild to moderate symptoms.
- Those with flexible deformities.
- Patients who want to delay or avoid surgery.
3. Symptomatic Flat Feet: Warning Signs to Watch For
When flat feet become problematic, they often present with:
⚠️ Areas of Pain & Dysfunction
- Medial arch pain due to tibialis posterior tendon strain.
- Heel pain from compensatory plantar fasciitis.
- Swelling along the inside of the ankle or foot.
- Weakness or fatigue during walking or push-off phase of gait.
Radiographic Signs of Progression
- X-rays: Collapsed medial arch, talar head uncovering, increased Meary’s angle.
- MRI: Degeneration of the tibialis posterior tendon, spring ligament laxity or early joint arthritis.
When to Seek Imaging:
- Persistent pain despite 3-6 months of conservative treatment.
- Visible or sudden changes in foot shape or arch height.
- Suspected tendon or joint involvement.

4. Risk Factors for Progression
Not all flat feet worsen over time, but some conditions increase the likelihood of progression:
High-Risk Indicators:
- Early and rapidly worsening pain.
- High body mass index (BMI), which increases mechanical stress.
- Lack of response to conservative care after 6+ months.
- Participation in high-impact sports (e.g. running, basketball).
- Trauma, or systemic ligament laxity syndromes like Ehlers-Danlos or Marfan.
Clinical Red Flags:
- Rigid flatfoot: Arch remains collapsed even when non-weight-bearing.
- Rapid progression: Noticeable changes on repeat imaging within months.
5. Minimally Invasive Surgical Options
When conservative treatments fail, surgical correction may be recommended, especially for patients with progressive pain or deformity. Newer minimally invasive techniques offer quicker recovery and less scarring.
A. Endoscopic Gastrocnemius Recession (Strayer Procedure)
- Releases tight calf muscle fibres to improve ankle flexibility and reduce arch strain.
- Outpatient procedure with relatively fast recovery.
B. Subtalar Arthroereisis
- A small implant is placed in the sinus tarsi to block excessive pronation.
- Best suited for flexible flat feet, especially in younger or active patients.
C. Minimally Invasive Calcaneal Osteotomy (MICO)
- Involves a small incision to shift the heel bone and correct alignment.
- Less invasive than traditional osteotomy, with faster healing and reduced downtime.
📚 A 2023 study in Foot & Ankle Surgery found that subtalar arthroereisis combined with gastrocnemius recession improved arch height and reduced symptoms in 85% of cases.
6. Return to Function After Surgery
Most patients regain near-normal function within 3-6 months after minimally invasive flatfoot correction.
Recovery Timeline:
- Weeks 1-6: Limited or protected weight-bearing, physical therapy begins.
- Months 2-4: Strength training and gait correction.
- Months 5-6: Return to higher-impact activities and sports.
📖 A 2022 Journal of Bone & Joint Surgery study reported 92% patient satisfaction at 1-year follow-up after MICO.
📖 A 2021 Foot & Ankle International paper found 80% of athletes returned to sport within 6 months after arthroereisis.
✅ Final Takeaway: When to Worry About Flat Feet?
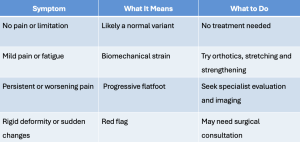
Bottom Line:
Flat feet only require treatment when they cause pain, dysfunction or progressive deformity. With timely intervention ranging from insoles and exercises to advanced surgical techniques, most adults can return to pain-free, active living. PRIME










Leave A Comment