Low back pain is one of the most common health complaints worldwide and a leading cause of disability, particularly among older adults. While many people accept back pain as an inevitable part of ageing, misunderstanding the causes and treatments can lead to unnecessary fear, inappropriate care, or delayed recovery.
Separating facts from myths is essential. With the right knowledge, most people can manage low back pain safely and effectively — and know when medical attention is truly needed.
What Is Low Back Pain?
Low back pain refers to discomfort, stiffness, or soreness felt in the area between the lower ribs and the buttocks, sometimes extending into the hips or legs. The pain may be sudden or gradual, mild or severe, and short-lived or persistent.
Although low back pain can affect people of all ages, its frequency and impact increase with age due to factors such as reduced muscle strength, degenerative changes in the spine, osteoporosis, and a higher risk of falls.

The Facts About Low Back Pain
Fact 1: Low Back Pain Is Common in Older Adults
Low back pain is extremely common. Global studies estimate that around one in five adults experience low back pain at any given time, with higher rates seen in older populations. As societies age, the number of people affected is expected to rise.
Importantly, most low back pain episodes are not dangerous and improve with time and appropriate self-care.
Fact 2: Most Low Back Pain Is “Non-Specific”
The majority of low back pain cases are classified as non-specific low back pain, meaning there is no single identifiable structural cause such as a fracture, infection, or tumour.
Non-specific pain is often related to:
-
Muscle strain or ligament stress
-
Reduced flexibility or muscle weakness
-
Poor posture or unaccustomed activity
-
Age-related wear and tear in the spine
Activities such as gardening, spring cleaning, lifting heavy items incorrectly, or long periods of sitting can trigger symptoms, especially in older adults who may be less physically conditioned.

Steps should be taken to prevent back strain at work
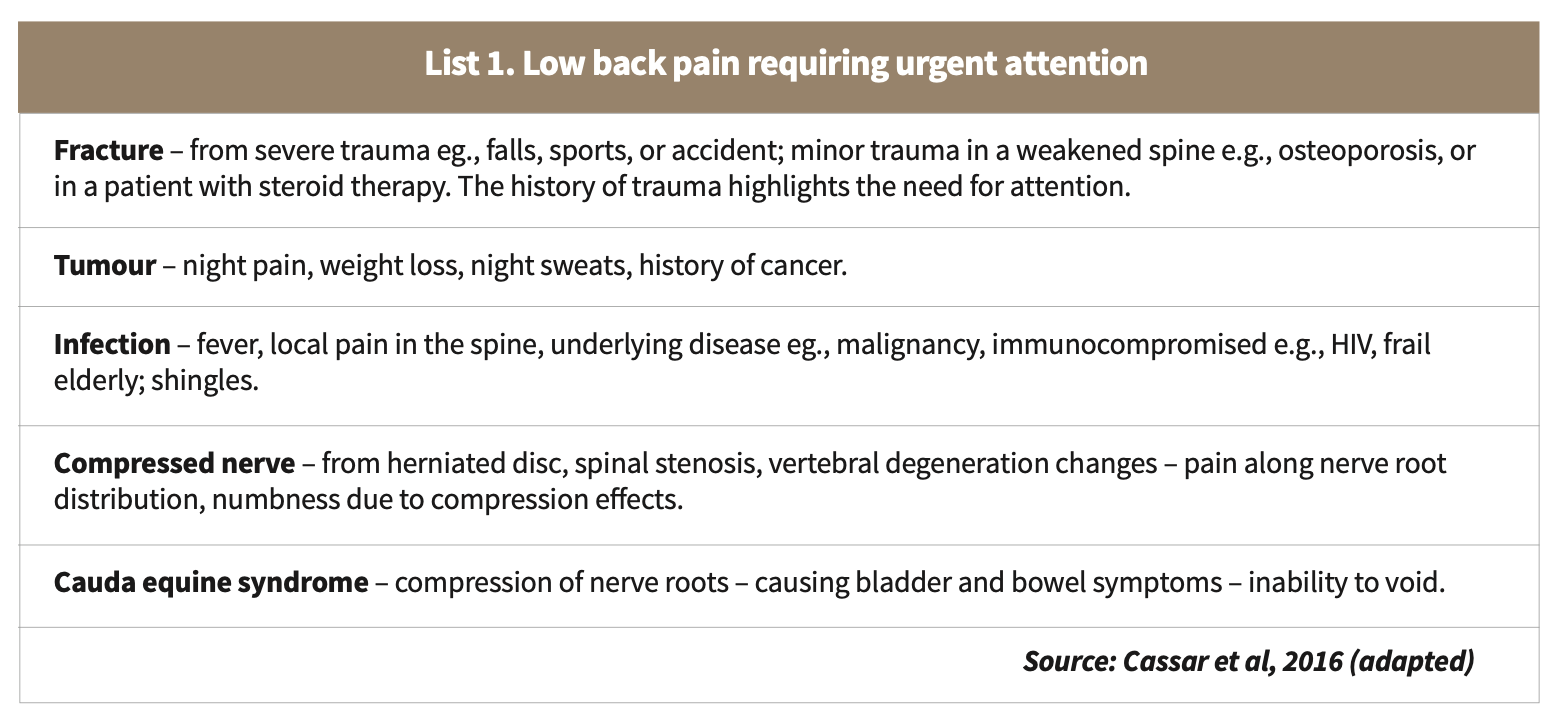
Fact 3: Some Causes Require Urgent Medical Attention
While most low back pain is benign, certain symptoms — often called “red flags” — may indicate a more serious underlying condition and require prompt medical assessment.
Red flags include:
-
Severe pain after a fall or injury
-
Unexplained weight loss
-
Fever or signs of infection
-
History of cancer
-
Progressive leg weakness or numbness
-
Loss of bladder or bowel control
Conditions such as spinal fractures, infections, tumours, severe nerve compression, or cauda equina syndrome are uncommon but serious and should not be ignored.
Fact 4: Low Back Pain Can Sometimes Come From Outside the Spine
Not all back pain originates from muscles or the spine. In some cases, pain felt in the lower back may be caused by extraspinal conditions, such as kidney problems, abdominal or pelvic disorders, or vascular disease.
Persistent pain that does not change with movement, or is associated with other systemic symptoms, should always be evaluated by a healthcare professional.
Fact 5: Preventing Back Strain Matters
Simple preventive measures can significantly reduce the risk of low back pain:
-
Safe lifting: Bend at the hips and knees, keep the back straight, and hold objects close to the body. Avoid twisting while lifting.
-
Movement breaks: Prolonged sitting or driving places strain on the lower back. Regular stretching and position changes help maintain spinal health.
-
Staying active: Gentle exercise strengthens muscles that support the spine and improves balance and flexibility.

Bodyweight has little relationship with low back pain
Common Myths About Low Back Pain
Myth 1: Everyone With Back Pain Needs X-Rays or MRI Scans
This is not true. Imaging tests are not routinely required for recent, uncomplicated low back pain. In fact, early imaging often does not improve outcomes and may lead to unnecessary worry.
Scans are usually reserved for:
-
Pain lasting more than six weeks despite appropriate care
-
Presence of red-flag symptoms
-
Suspicion of serious underlying disease
Myth 2: Bed Rest Is the Best Treatment
In the past, bed rest was commonly advised. Today, we know that prolonged rest can delay recovery.
Most guidelines recommend:
-
Staying as active as pain allows
-
Avoiding prolonged bed rest
-
Gradually returning to normal activities
Gentle movement promotes healing, maintains muscle strength, and reduces stiffness.
Myth 3: Painkillers Alone Are the Answer
Simple pain relief, such as paracetamol, may help with mild pain, particularly in older adults. However, medication works best when combined with movement, education, and self-care strategies.
Pain relief should support activity — not replace it.
Myth 4: Body Weight Has Little to Do With Back Pain
This is false. Excess body weight increases mechanical stress on the spine and is associated with a higher risk of low back pain and sciatica, especially in older adults.
Studies show that managing body weight through regular physical activity and balanced nutrition may reduce the risk of developing nerve-related back pain.
When Should You See a Doctor?
You should seek medical advice if:
-
Pain is severe or worsening
-
Symptoms last longer than a few weeks
-
There are red-flag symptoms
-
Pain significantly limits daily activities
Early assessment helps rule out serious conditions and provides reassurance and guidance.
Conclusion: Knowledge Empowers Better Back Care
Low back pain is common, especially as we age, but it does not have to lead to fear or inactivity. Understanding what is normal, what is not, and how to respond appropriately allows individuals to manage symptoms confidently and safely.
Most low back pain improves with time, movement, and sensible self-care. By replacing myths with facts, older adults can remain active, independent, and resilient — even in the face of back pain. PRIME