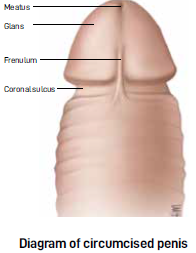
Male circumcision is the surgical removal of the penile prepuce, more commonly known as the foreskin. The earliest known circumcision dates back to the prehistoric era. Around the world, circumcision is frequently performed on children as part of religious requirements, such as in Judaism and Islam. About 30% of remaining circumcisions are performed for sociocultural practices and non-religious reasons.
REASONS/BENEFITS OF CIRCUMCISION
The most common reasons for circumcision in adults are phimosis, balanitis/balanoposthitis or dyspareunia (painful intercourse). There are significant variations in rates of circumcision globally. The circumcision rate in the United States (US) is as high as 80%, while other countries report a circumcision rate of only 0.1 %. The high rates of circumcision can be due to historical and sociocultural reasons. Aesthetics and cosmesis are popular reasons for adult circumcision in specific communities.
There is conflicting research on whether circumcision may help to prevent penile cancer. The rationale for this research is based on the observation that penile cancer appears to occur exclusively in uncircumcised men. However, in-depth analysis revealed that circumcision is only helpful if it is performed early in life.
Several high-quality studies have shown that circumcision reduces the risk of HIV infection by 60% as well as the transmission of some sexually transmitted infections (STIs). As a result, global guidelines recommend circumcision in countries with high incidences of HIV. It is important to remember that circumcision alone is not effective in reducing HIV infections. It needs to be complemented with education, protective measures, and the avoidance of high-risk behaviours.
To better understand medical circumcision, we need to rewind to the early days of a baby boy. Circumcision for religious reasons is usually performed early in a baby’s life. It is commonly performed in the first week of life, early childhood, or the prepubertal period. For this article, we will cover only medically indicated circumcision.
NON-RETRACTABLE FORESKIN
Only 4% of babies have a retractable foreskin. The percentage increases to 50% by the first year of life, and goes up to 89% by the age of three. Up to 10% of the young male population may have foreskin issues.
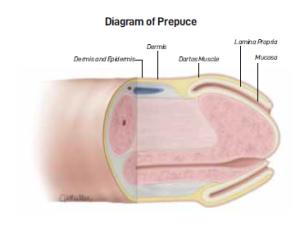
Non-retractile prepuce must be considered if there are no other urinary symptoms like pain or swelling. Preputial adhesion can also prevent the foreskin from being retracted. As the child grows, the adhesion separates the inner foreskin from the glans (head) of the penis.
Epithelial debris (dead skin cells) called smegma can accumulate within the foreskin. Together with penile erection, they help encourage adhesion to separate in a growing child. Increased smegma production coincides with puberty when most boys can retract their foreskin.
Occasionally, smegma collection occurs in a nodule form and can be mistaken for a cyst. Smegma can be mixed with urine, leading to a purulent-like discharge which can be confused with an inflammatory condition called balanitis. Parents must understand that their children may have a non-retractable foreskin, which is a normal phenomenon. Forceful retraction of the foreskin in young children for cleaning purposes is often unnecessary and causes pain. It can cause scar formation and result in the formation of secondary phimosis.
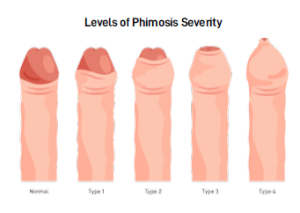
PHIMOSIS
Phimosis refers to the inability to retract the foreskin below the glans of the penis. This is commonly due to a narrow ring along the foreskin. Phimosis is estimated to occur in 9-20% of boys between the age of 5-13. It is important to differentiate between phimosis (mechanical tightening) and preputial adhesion in the non-retractile foreskin, which can be tricky. Ballooning of the penis can occur during voiding due to adhesion or phimosis, and may be physiological (normal development). It is not a recognised indication for circumcision.
MEDICAL CONDITIONS REQUIRING CIRCUMCISION
We now move on to the medical conditions where circumcision may be required.
- Paraphimosis
Phimosis can lead to paraphimosis where the retracted foreskin becomes trapped and cannot pull up. The narrow ring of the foreskin can constrict the blood flow in the penis leading to pain, discomfort and potential organ damage. Paraphimosis is a medical emergency and should be attended to immediately.
- Balanitis/Balanoposthitis
Balanitis/balanoposthitis is the infection of the glans/foreskin respectively. These are two conditions which
parents of young boys need to be aware of as their children may complain of pain with swelling around the penis, which can occur with pus. Balanitis/balanoposthitis can be caused by exposure to an irritant like a new brand of soap or excessive cleaning. Non-specific balanitis/balanoposthitis can be treated with topical antibiotic ointment.
- Balanitis Xerotica Obliterans (BXO)
This is a non-painful chronic inflammatory condition that affects the glans, foreskin, meatus and urethra. It is characterised by white atrophic plaques on the glans, which coalesce into a sclerotic lesion. It is uncommon in children and is more commonly found in adults. Determining the cause of the narrow foreskin is crucial before deciding on the course of treatment. It is important to understand that circumcision is not the only option for foreskin issues. The first-line treatment for phimosis is topical steroids. Research shows that topical steroids given twice daily for 4-8 weeks can improve phimosis up to 80% of the time, while effective, long-term administration of steroids is not recommended as it can result in skin thinning. As such, recurrence of phimosis occurs in 20% of cases after the stoppage of steroids.

Circumcision may be necessary when phimosis does not respond to steroid treatment or when there is repeated balanitis/balanoposthitis in children. In such cases, circumcision can solve the issue once and for all. In paraphimosis, the foreskin should be replaced to its original position as soon as possible before circumcision. Early reduction of paraphimosis reduces discomfort. Reduced tissue swelling results in better cosmesis during circumcision.
In children with recurrent attacks of urinary tract infection or congenital urinary tract abnormalities, circumcision has been shown to help reduce bacterial colonisation at the glans, with a resultant reduction in urinary tract infections.
POINTS TO NOTE
There are many ways to perform circumcision. The techniques can be broadly classified into preputioplasty (partial removal of the foreskin) and circumcision. There are different methods of circumcision in children and adults, which we will not cover in this article. It is best to discuss the optimal way of performing circumcision with your urologist. Also, circumcision is contra-indicated (should not be performed) in foreskin that is infected, and for children with congenital abnormalities like hypospadias or curvature of the penis(chordee) as the foreskin can be used for reconstruction later in life.
CONCLUSION
Circumcision is a common procedure that is performed on both children and adults. Ultimately, there are many reasons why circumcision may be performed. Circumcision may be influenced by sociocultural, religious, personal preference, local expertise or medical indications. It is important to understand the indication for surgery and the potential complications that can occur with this surgery. It is also important to note that circumcision should be performed for clear indications as complications like bleeding, infection and wound dehiscence, while rare, can occur complications that can occur with this surgery. It is also important to note that circumcision should be performed for clear indications as complications like bleeding, infection and wound dehiscence, while rare, can occur.
Key Take Home Points
- Forceful retractable of the foreskin in young children
for cleaning is unnecessary and causes pain. Force
retraction of foreskin can cause scar formation and
secondary phimosis.
- Ballooning of the penis during voiding may be
physiological and is not a recognised indication
for circumcision.
- Circumcision is not the only option for foreskin issues.
- Circumcision should be performed for clear indications as complications like bleeding, infection and wound dehiscence, while rare, can occur.
Dr Jay Lim
Consultant Urologist
PanAsia Surgery Group
MBBS (U of Sydney, Australia)
Dr Jay Lim is a Consultant Urologist at PanAsia Surgery Group. Before joining PanAsia, Dr Lim was trained at SGH and had a fellowship in robotic surgery at Macquarie University, Sydney, Australia. He was the first doctor to be appointed Principal Medical Investigator by Artificial Intelligence Singapore, and he was the Director of the Urology Cancer Registry (UroCaRe). Dr Lim specialises in kidney stone diseases, including acute renal colic; horseshoe kidneys; and pregnancy-related, stonerelated
and single kidney patients. He is trained in the full spectrum approach for large and small renal stones, including endoscopic, laparoscopic and ultrasound-based supine percutaneous techniques for large stones.

Mount Elizabeth Novena
Specialist Centre
38 Irrawaddy Road #10-43/44
Singapore 329563
Call: +65 6570 2608
Whatsapp: +65 9677 7940
Website: www.panasiasurg.com