Everything you need to know about COPD
Chronic Obstructive Pulmonary Disease (COPD) is a lung disease that is characterized by chronic (long-term and progressive) airflow into and out of the lungs, such that it interferes with normal breathing. This is caused by destruction of lung tissue where oxygen is exchanged. The result is reduced oxygen absorbed and difficulty removing carbon dioxide, the body’s waste gas. COPD is sometimes called emphysema (destruction of the gas-exchanging surfaces of the lungs) or chronic bronchitis (persistent cough and sputum production for at least 3 months in 2 consecutive years).
COPD is the 4th leading cause of death in the world and is projected to become the 3rd leading cause of death in 2020. The prevalence and burden of COPD are projected to increase due to greater exposure to COPD risk factors and the world’s ageing population, with more people experiencing the long-term effects of COPD. This can lead to a significant increase in disability and mortality around the world, contributing to years lost due to premature mortality and years living with disability. This is unfortunate as COPD is both preventable and treatable.
What Causes COPD?
COPD is caused by long-term exposure to irritants that damage your lungs and airways. The main cause of COPD worldwide is cigarette smoking. Pipes, cigars and other types of tobacco smoke (e.g. shisha smoking) can also cause COPD. The more cigarettes you consume, the higher your chances of developing COPD. This results from complex interaction between the genes and the environment irritants. Passive exposure to cigarette smoke (called environmental tobacco smoke) may also contribute to COPD development.

Other causes of COPD include exposure to second-hand smoke, air pollution, chemical fumes or dusts, or combustion of biomass (cooking with plant/animal material) in an enclosed space. This is usually encountered in underdeveloped countries. In rare cases, a genetic condition called alpha-1 antitrypsin deficiency (AAT deciciency) can play a role in causing COPD as well. Patients with this disorder usually develop symptoms of COPD younger, between 20-50 years old. It is uncommon in people of Asian descent.
What are the Symptoms of COPD?
In the very early stages of COPD, there may be no symptoms, but as the disease gradually worsens, symptoms such as shortness of breath during physical activity (and eventually, at rest) manifests. Other common symptoms include a persistent cough that produces mucus, tightness in the chest or wheezing (a high-pitched whistling sound in the chest during breathing). Initially, these symptoms may be transient and disappear after a period of treatment, but gradually, they become more persistent with shorter intervals between each episode.
Some diseases, such as asthma, congestive heart failure and lung infections, may mimic the symptoms of COPD. As such, it is important to obtain an early correct diagnosis of COPD.
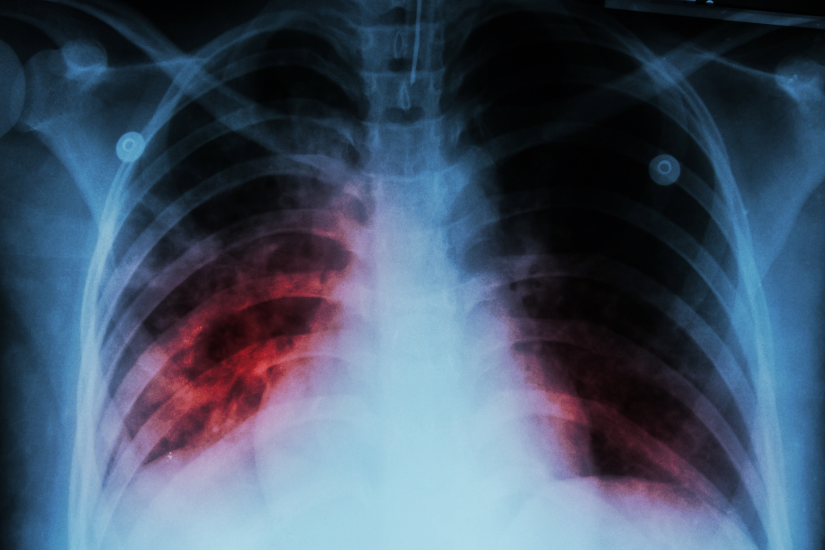
How is COPD Diagnosed?
COPD is diagnosed by performing a spirometry, a simple painless office-based test which measures how deeply a person can breathe and how fast air can move in and out of the lungs.

So What If I Have COPD?
Once you have been diagnosed with COPD, the disease is usually progressive, with symptoms of coughing getting worse over time. The disease is also punctuated by excerbations of COPD that are characterized by increased coughing, wheezing and shortness of breath, which can be caused by a virus or bacterial infection, or by exposure to inhaled irritants. These episodes can be frightening as one would feel that there is not enough air getting into the lungs. This has been described as being like a drowning episode. Some patients require hospitalization for treatment, while those with a severe attack might even require ICU admission and assistance with breathing.

Having COPD also puts you at risk of other medical conditions, such as pneumonia, pulmonary hypertension (high blood pressure in the arteries supplying blood to the lungs), lung cancer, heart disease (heart attacks, heart failture and irregular heart beats), diabetes, osteoporosis and depression.
The COPD Assessment Test™ (CAT™) is a simple and quick questionaire that measures the health status impairment in COPD. It can help physicians determine the severity of COPD and the appropriate treatment that can be offered.
How can I Prevent or Treat COPD?
There is no cure for COPD, but it is possible to slow the progress of the disease, reduce symptoms and minimize exacerbations. An early diagnosis is key to establishing the right treatment. Lifestyle changes, such as quitting smoking and avoiding pollutants, are key. Medications, such as inhaled brochodilators (drugs that open the air passages), can relieve breathlessness, reduce cough and phlegm production, and allow improvement in health status. Vaccinations are important to reduce susceptibility to infections.
It is important to also maintain a healthy lifestyle, such as exercising regularly and minimizing consumption of processed foods as these can worsen decline of lung function. A healthy diet should minimize carbohydrate intake and include a “Mediterranean diet” consisting of food with antioxidant and antiinflammatory properties.

When you experience an exacerbation of COPD (increased sputum quantity or colour, increased cough with fever and shortness of breath), you should seek treatment as soon as possible with your doctor. Antibiotics, steroids and medications to open the air passages (bronchodilators) are usually needed. In some instances, admission to hospital might be needed to treat such exacerbations, which sometimes can take a few days to recover. But after an exacerbation, it is common to feel lethargic and many patients experience a significant drop in effort tolerance for an extended period of time. Hence, preventing an exacerbation is important.
Article by

Dr Steve Yang
Consultant
The Respiratory Practice
Dr Yang obtained his basic medical degree from the National University of Singapore in 1994, and subsequently received training in Respiratory Medicine and Intensive Care Medicine at Singapore General Hospital (SGH). He further trained in Intensive Care Medicine and Interstitial Lung Disease at the University of Washington Medical Centre in Seattle, USA. He has obtained his Fellowship with the College of Chest Physicians (USA), the Chapter of Respiratory Physicians (Singapore) and the Chapter of Intensive Care Physicians (Singapore). He also holds the European Diploma in Intensive Care. Dr Yang is currently a Consultant in The Respiratory Practice and has a strong interest in Critical Care, Interstitial Lung Disease as well as End-stage Lung Diseases. He is involved with research in Critical Care and Interstitial Lung Disease, and has published in both local and overseas medical journals.
https://www.respiratorypractice.com/
Phone: 6256 2606
820 Thomson Road,
#06-56 Mount Alvernia Medical Centre D
Singapore 574623











