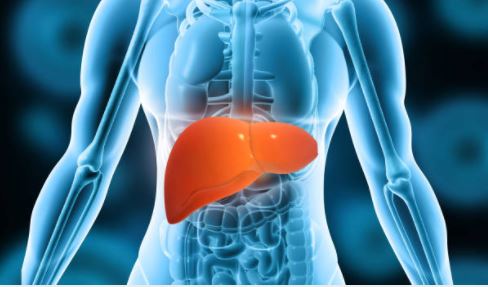
Liver cancer is cancer that develops primarily in the liver. It is important to differentiate primary liver cancer from cancer metastasized from other parts of the body. Liver cancer usually occurs in patients with chronic inflammation or infection of the liver. There are several types of liver cancers, with the main type being hepatocellular carcinoma (HCC).
A COMMON CANCER
According to the World Health Organisation International Agency for Research on Cancer (IARC), liver cancer is the 5th most common cancer diagnosed in Singapore in 2020, alongside breast cancer (3,662 cases), colorectal cancer (3,558 cases) and lung cancer (2,916 cases) – the top three cancers diagnosed in Singapore for both genders and all ages. Locally, there were about 3.7 cases of liver cancer diagnosed each day in 2020. They were more commonly diagnosed in males than females. Even though liver cancer is only the 5th most common cancer in Singapore, it is actually one of the top three leading causes of cancer deaths for males in Singapore from 2014 to 2018.
RISK FACTORS
Most primary liver cancer cases (HCC) diagnosed globally are due to chronic hepatitis B infection, while the rest are diagnosed based on pre-existing conditions of liver cirrhosis (hardening of the liver due to longstanding inflammation and scarring). It is important to recognize the underlying causes early. This can be done by screening for common liver conditions, such as hepatitis B and hepatitis C infections, and for fatty liver that can lead to liver cirrhosis, which is one of the biggest risk factors for liver cancer development. Other important risk factors for liver cancer include chronic hepatitis B, a family history of liver cancer, smoking and excessive alcohol use. When the underlying condition is diagnosed early and the patient is given timely treatment, the chances of development into liver cancer would be greatly reduced. Among the top ten types of cancers, liver cancer has one of the poorest survival rates. The main reason for this is because by the time of diagnosis, a lot of liver cancer patients already have late-stage disease. This is because liver cancer usually starts insidiously; in early stages, patients would not have any symptoms and thus, are unlikely to seek medical attention. Commonly, most people who carry hepatitis B or C infections do not realise that they have the condition or even liver cirrhosis for many years. Therefore, liver screening is needed to detect these underlying liver conditions which predispose the individual to liver cancer. Regular screening, including blood tests and ultrasound scans, are required to detect the cancers early. Anyone with a family history of hepatitis B or C, or liver diseases, should also seek medical attention early.
REDUCING RISK FACTORS
So what are the things that we can do to reduce the risk factors for getting liver cancer? There are three main areas we can look at. They are:
• Maintaining a healthy lifestyle
• Early medical screening for risk factors
• Control of underlying cause, which will minimise risks and help to get the condition diagnosed early
MAINTAINING A HEALTHY LIFESTYLE
It is important to maintain a healthy body weight and avoid development of fatty liver. Obesity and diabetes will increase the risk of liver cancer by two to three-fold if you have existing liver conditions like hepatitis B or C. Studies have shown that regular exercise and a few cups of coffee a day will reduce your lifetime risk of liver cancer development.
EARLY SCREENING
If you have family members with a medical history of chronic hepatitis (such as hepatitis B) or liver cancer, you should seek medical attention and screen for risk factors of liver diseases and liver cancer. The main risks for chronic liver diseases in Singapore are chronic hepatitis B infection, chronic hepatitis C infection, obesity/diabetes leading to fatty liver, and excessive alcohol intake. Your doctors can screen you for these conditions and perform liver scans to exclude liver cirrhosis. Once any condition that causes chronic liver disease is diagnosed, regular follow-up with your gastroenterologist will enable early treatment of liver inflammation related to the condition. For example, liver inflammation related to chronic hepatitis B can be treated before the condition worsens and progresses to liver cirrhosis. If you end up having liver cirrhosis or chronic hepatitis B, your doctor will also do regular blood tests and ultrasound scans to screen for any lesions that may be early signs of liver cancer. This is because liver cancer does not cause any symptoms in a person until the late stage. By that stage, treatment for the liver cancer will be limited.
MEDICAL CONTROL OF UNDERLYING CONDITIONS
Following up with your gastroenterologist will allow you to receive necessary treatment early. Currently, there are potent drugs that can be used against chronic hepatitis B and hepatitis C infections. These significantly reduce the risk of liver cancer development by suppressing the virus, and ultimately cure the condition. Tenofovir alafenamide (TAF) is a potent anti-hepatitis B drug that can reduce the risk of liver cancer and cirrhosis development by 50-80% over time. Sofosbuvir/Velpatasvir is another potent drug that can cure chronic hepatitis C infection with a 98% success rate after only 3 months of treatment. These drugs can effectively reduce the future risk of liver cancer and liver cirrhosis progression. Patients with fatty liver can reduce the progression to cirrhosis by getting evaluation from the liver specialists. Healthy lifestyles must be maintained to reduce body weight and the risk of disease progressing to cirrhosis.
DIAGNOSIS
In general, patients with certain chronic liver conditions (such as hepatitis B) who are at risk of developing liver cancer should have follow up with their family doctors or liver specialists, and go for regular blood tests and ultrasound scans of the liver once every 6-12 months. People with chronic liver conditions that run a higher risk of developing liver cancer, such as liver cirrhosis and chronic hepatitis B on treatment, should get ultrasound liver scans and blood tests done once every six months. If a routine scan detects liver nodule(s) that is suspected for liver cancer, the doctor will usually perform another scan, such as CT or MRI, on the liver to further improve diagnostic accuracy and confirm whether the nodule is liver cancer.
TREATMENT
There are several liver cancer treatment options available, but the treatment decision largely depends on the size and location of the tumour, and whether there are single or multiple lesions within the liver. These considerations are in addition to the person’s overall health status. If the tumour is small and at a location that is easily accessible, the doctor may recommend surgery to remove the tumour or use radiofrequency ablation to “burn off” the cancer. Another treatment that is less common but provides excellent outcome is liver transplantation. In some cases where the liver cancer is not ideal for the above treatment options, the doctor may recommend a procedure called “transcatheter arterial chemo-embolization” (TACE) to shrink the tumour, with an intent to kill the cancer with chemotherapy agent while closing off the artery that supplies the tumour. Sometimes, this treatment may only shrink the tumour temporarily over the next 3-6 months. Hence, for this procedure, patients will require a number of sessions over 6-12 months to ensure the liver cancer is adequately treated. Finally, when the liver cancer is more advanced but the liver still retains good function, the doctor may recommend drug therapy with targeted drugs to control the liver cancer. There are also newer specific antibody treatments available that can target the immune system to allow clearance of the tumours. However, these agents will require close monitoring by the oncologist.
TAKING CARE OF THE FAMILY
If you have any family members who have been diagnosed with chronic hepatitis B, it is important to go to your doctor and request for hepatitis B screening tests for everyone in the family. This is particularly necessary for a pregnant mother as there is a possibility that hepatitis B infection can be passed on to the child at birth. This is known as vertical transmission. As hepatitis B vaccination was only available in Singapore from the late 1980s, those who were born before this period should have their hepatitis B antibodies checked at their family doctors. If you have other conditions that predisposes you to advanced liver diseases such as fatty liver and excessive alcohol intake, it is recommended to talk to your doctor regarding this.
In conclusion, awareness of the causes leading to high liver cancer risk is important. Early diagnosis and intervention of these liver conditions can reduce your liver cancer risks for many years to come.
Dr John Hsiang
Dr Hsiang is an established gastroenterologist at Livingstone Health with more than 15 years of clinical experience. He has been caring for both local and expatriate communities, and is well regarded for his professional and caring demeanour. Dr Hsiang graduated from Otago Medical School, New Zealand in 2003 and completed his specialist training in 2012. In 2013, he furthered his research career and post-specialist training in the Chinese University of Hong Kong, under world-renowned Professor Henry Chan, Professor Vincent Wong and Professor Grace Wong. Dr Hsiang has published many peer-reviewed studies on a variety of topics including hepatitis B, obesity related liver disease, hepatitis C, gut microbiome, liver cirrhosis, helicobacter infection and alcoholic liver disease. He is fluent in Mandarin, English and Hokkien.