
Sugar & Smiles | Understanding How Diabetes Affects the Mouth and Gums by Dr Raymond Lim
Diabetes mellitus refers to a group of metabolic diseases that cause high blood glucose levels (hyperglycaemia). This occurs when the body does not make enough insulin, does not make insulin at all, or cannot use insulin effectively. As diabetes is common, dentists often see patients who live with this condition.
There are two main types of diabetes.
-
Type 1 diabetes is a chronic autoimmune disease. The pancreas produces little or no insulin. This type accounts for about 5–10% of all diabetes cases.
-
Type 2 diabetes is much more common, making up 85–90% or more of cases. In type 2, the body’s tissues respond less effectively to insulin, insulin production becomes irregular, or both happen together.
How Uncontrolled Diabetes Can Affect the Mouth
When blood sugar is not well-controlled, it can lead to several oral symptoms, such as:
-
Dry mouth (reduced saliva flow)
-
A burning sensation in the mouth
-
Slow or delayed healing
-
Increased risk of infections
-
Oral candidiasis (fungal infection)
-
Swelling of the parotid salivary glands
-
Gingivitis (gum inflammation)
-
Periodontitis (advanced gum disease)
Patients with diabetes are often familiar with the signs of low blood sugar (hypoglycaemia) and may manage symptoms early. However, dental staff should also know how to recognise and treat hypoglycaemia. Using a glucometer to check blood glucose levels is important. Every dental clinic should also have a clear protocol for assisting patients, both when they are conscious and when they are unconscious.
Diabetes, Smoking, and Gum Health
Both diabetes and smoking increase the risk of periodontitis. There is some evidence that having both factors together may increase this risk further. The exact reasons are not fully clear. Studies comparing people with diabetes who smoke and those who do not show inconsistent findings in the oral microbiome, the inflammatory response, and periodontal health.
Periodontal Treatment and Glycaemic Control
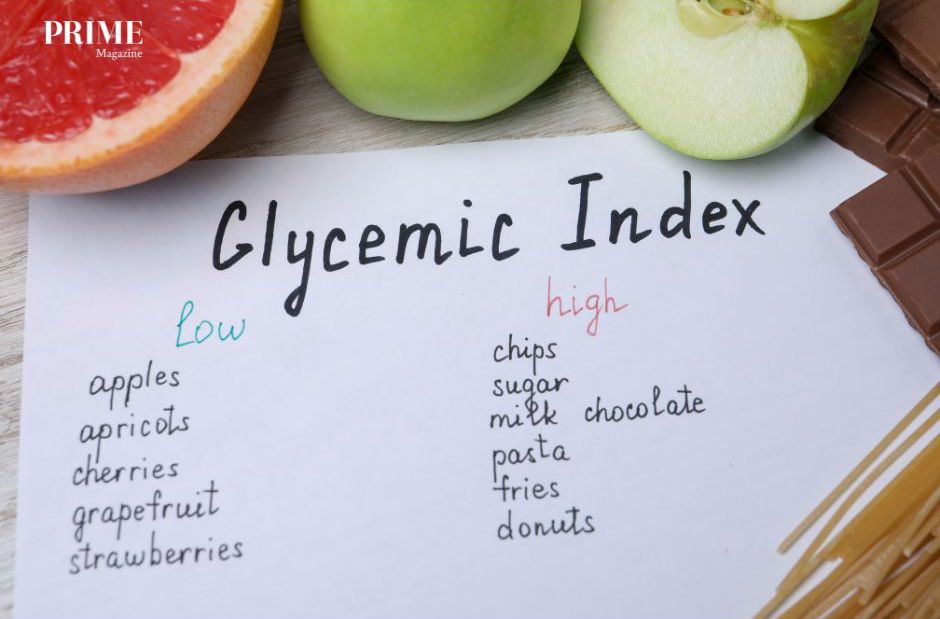
Glycemic Index
There is ongoing interest in how periodontal treatment may influence glycaemic control.
-
A 2018 systematic review of observational studies found insufficient evidence to assess the impact of periodontitis on glycaemic control in people with type 1 diabetes. However, it noted that type 2 diabetes patients with periodontitis tended to have higher HbA1c levels and more diabetes-related complications.
-
Another 2018 systematic review of randomised controlled trials found that scaling and root planing significantly reduced HbA1c levels at three months, with further improvement at six months.
However, not all studies agree:
-
A 2013 study on patients with type 2 diabetes did not find an improvement in glycaemic control after periodontal treatment.
-
A 2018 study reported no significant change in glycaemic control in patients with either type 1 or type 2 diabetes after treatment.
Although the evidence is mixed, most experts agree that patients with diabetes benefit from periodontal therapy, especially when it is paired with consistent oral care at home. PRIME










Leave A Comment