Importance of Breast Screening and How it Can Affect Your Life.
A mother of two in her 40’s once said to me when she entered my consultation room: “I think it is…I didn’t think it was anything, but now I think it is serious.”
The changes in her breasts from the progression of cancer was obvious over the course of one year since she first noticed a painless lump.
“I am also more breathless now when I walk.”
Sadly, the cancer had already spread to other parts of her body.
Are many of us taking our lives for granted? Why do we not take the initiative to take up preventive measures, such as screenings? How can we take care of our breast health and is there a point in doing so?
 Every October, pink ribbon efforts to raise awareness surrounding breast cancer abound globally. Major landmark buildings in different countries light up in pink and departmental stores feature pink products. Various advocacy groups and activist individuals, including celebrities, athletes, survivors and family members, dress in pink or wear the breast cancer pin as they conduct/participate in various breast cancer awareness events and campaigns. All these for a very good reason – to save lives.
Every October, pink ribbon efforts to raise awareness surrounding breast cancer abound globally. Major landmark buildings in different countries light up in pink and departmental stores feature pink products. Various advocacy groups and activist individuals, including celebrities, athletes, survivors and family members, dress in pink or wear the breast cancer pin as they conduct/participate in various breast cancer awareness events and campaigns. All these for a very good reason – to save lives.
Breast cancer awareness is incredibly important because early detection – often through screening – can catch the disease when it is most treatable. A heightened awareness of the disease has unquestionably led to a greater number of women being screened for breast cancer. This has translated to better outcomes for the patients and reduced breast cancer mortality rate, because of the earlier diagnosis and state-of the-art treatment options available to them. With greater awareness, the public is also better educated on the potential impact of breast cancer and how they can take personal responsibility towards their health.
FACTS ABOUT BREAST CANCER
 Breast cancer is a significant public health problem across the world. In Singapore, it is the most common female cancer and the No. 1 cause of cancer-related death in women. It is estimated that 1 in 15 women in Singapore will develop breast cancer in their lifetime; in the USA, this figure is 1 in 8. And if you think that breast cancer is an exclusively female disease, you are mistaken. Although much less common, breast cancer affects men too.
Breast cancer is a significant public health problem across the world. In Singapore, it is the most common female cancer and the No. 1 cause of cancer-related death in women. It is estimated that 1 in 15 women in Singapore will develop breast cancer in their lifetime; in the USA, this figure is 1 in 8. And if you think that breast cancer is an exclusively female disease, you are mistaken. Although much less common, breast cancer affects men too.
The majority of breast cancer occurs sporadically. This means that it can occur in a person without known genetic mutation or family/personal history of cancer. Early detection remains the cornerstone of breast cancer control. When breast cancer is detected early, and patients undergo timely and effective treatment, they have the best chance of beating the disease. Indeed, early diagnosis and timely treatment is key to reducing the death toll associated with breast cancer.
SIGNS AND SYMPTOMS
 There are usually no signs or symptoms when the cancer begins. In the early stage, the patient looks and feels normal. However, as the cancer progresses, symptoms and signs will appear. Not all breast cancer symptoms present in the same way. Signs of breast cancer may include the following:
There are usually no signs or symptoms when the cancer begins. In the early stage, the patient looks and feels normal. However, as the cancer progresses, symptoms and signs will appear. Not all breast cancer symptoms present in the same way. Signs of breast cancer may include the following:
1. A hard and usually painless lump in the breast or underarm;
2. Swelling or thickening/hardening in part or all of the breast;
3. Dimpling of breast skin;
4. Redness, scaliness or rash of the nipple or breast skin;
5. Changes in size or shape of the nipple and breast;
6. Nipple discharge; and
7. Localised, persistent breast pain.
While it is important for a woman to know how her breasts normally look and feel, as well as the changes to look out for, she should still get her regular mammograms and clinical breast exams done as these tests can help detect breast cancer before symptoms appear.
RISK FACTORS
The main risk factors for developing breast cancer include:
1. Gender (Being a woman);
2. Age (Risk increases with age);
3. Having longer menstrual period history; and
4. Having personal/family history of breast cancer and carrying mutated breast cancer genes.
Although these risk factors cannot be changed, women should still make an effort to take note of their family history. Women with a family history of breast, ovarian, melanoma or pancreatic cancer may be at increased risk. They should talk to their doctors about possible genetic testing and when they should begin screening.
 There are also other risk factors which are lifestyle-related. These include drinking alcohol, being overweight, not being physically active, taking prolonged courses of birth control pills or hormone therapy after menopause, and not having children. For these risk factors, women have the choice to make healthy lifestyle decisions that can lower the risk.
There are also other risk factors which are lifestyle-related. These include drinking alcohol, being overweight, not being physically active, taking prolonged courses of birth control pills or hormone therapy after menopause, and not having children. For these risk factors, women have the choice to make healthy lifestyle decisions that can lower the risk.
In order to lower the risk of breast cancer, you may try to:
1. Attain and maintain a healthy weight by balancing your food intake with physical activity to avoid excess weight gain;
2. Be physically active; and
3. Limit or avoid alcohol altogether as risk increases with the amount of alcohol consumed
It should be noted that greater risk is tied to factors such as body weight, dense breast tissue, personal health history, family history or known gene mutations.
BREAST CANCER SCREENING
There are three tests typically used to evaluate breast changes and detect breast cancer. Each has its benefits and risks. Your doctor will recommend the modality best suited to you based on several factors, including your individual risk profile. The three most common tests are:
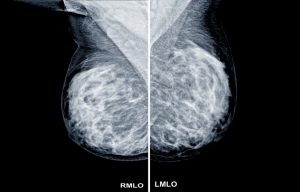
1. Mammogram – It is an x-ray exam of the breast. Its ability to detect cancer depends on several factors, including tumour type, size, and breast tissue density. In dense breasts, the conventional 2D mammogram may not detect small tumours as the overlapping breast shadows can hide them. Tomosynthesis, AKA 3D mammogram, has been shown to be able to detect more cancers in ladies with dense breasts as compared to the conventional 2D mammogram. When going for 3D mammogram, compression is the same as in 2D mammogram, but the technology captures multiple images of the breast using very low radiation doses to recreate the 3-dimensional picture of the breast. It has been shown to be safe and helps to reduce false alarms.
2. Ultrasound – Breast ultrasound is often used alongside mammography for women with dense breast tissue. It is also used for high-risk women who cannot undergo MRI.
3. MRI – A breast MRI (Magnetic Resonance Imaging) is used to screen high-risk women and to gather more information about a suspicious area found on a mammogram or ultrasound.
IMPORTANCE OF SCREENING
The truth is that no one really knows which one of us will get cancer and which type of cancer we may get. Regular breast screening can help to detect breast cancer when it is still early, when signs and symptoms are absent. In summary, when cancer is detected early, the chances of survival are greater.
RECOMMENDATIONS
Although there is no sure way to prevent breast cancer, you can make smart lifestyle choices to avoid the known risk factors and aim at early detection by going for age-appropriate screening. Breast self-examinations are important and women can begin to start getting familiar with their breasts beginning at the age of 18. At 40, women should begin screening for breast cancer. For women with higher risks of breast cancer, they should decide if they want to have a risk assessment at the age of 30, instead of 40.
IMPORTANCE OF BREAST CANCER AWARENESS
 Breast cancer awareness can change your perspective on your health, and allow you to take charge and be more responsible for your own health. To conclude, let’s revisit the many reasons why it is important to be informed and aware of breast cancer.
Breast cancer awareness can change your perspective on your health, and allow you to take charge and be more responsible for your own health. To conclude, let’s revisit the many reasons why it is important to be informed and aware of breast cancer.
Breast cancer is, by far, the most common cancer in women worldwide. Furthermore, it is deadly. Do not think that it cannot happen to you. And do not ignore changes you notice in your breasts – get them checked.
Risk factors are elements that increase your likelihood of developing breast cancer. The major contributors to increased risk are gender (being a women), having genetic mutations and certain lifestyle choices. Identify your risk factor and choose good lifestyle choices to lower your risk by eating healthy, avoiding alcohol and exercising regularly.
Know your risk factors: if there is significant family history, a genetic testing may be performed and screening can start at a younger age.
Early detection is possible through screening.
Even if you have no signs, you should still go for regular screenings because the early stages of cancer usually produces no symptoms or signs.
Detecting cancer at an earlier stage allows for more effective treatment and saves lives.
Women in their 20s do get breast cancer; however, the risk is higher for women above the age of 40. Women at this age should seriously consider getting screened once a year with mammogram and/or ultrasound (for dense breasts).
Men, though less common, can also get breast cancer.
Know how your breasts look and feel, and regularly perform breast self-examinations (monthly) to keep yourself aware of any changes to your breasts.
Lower prescriptive hormone replacement therapy after menopause has led to gradual reduction in female breast cancer incidence rates among women aged 50 and older.
Death rates from breast cancer have been declining, in part due to increased awareness, better screening and early detection, and continually improving treatment options.
Breast cancer awareness month in October every year helps the public to understand the importance of early detection and treatment. Lack of awareness on early detection and its impact on the health and life of individuals often results in women being diagnosed with breast cancer in late stages.
 Dr Jendana Chanyaputhipong
Dr Jendana Chanyaputhipong
General Surgery (Breast)
Dr Jendana received the Degrees of MB, MCh, BAO (Ireland, Hons) in 2004 and completed her Advanced Specialist Training in General Surgery in Singapore. She obtained her FRCSEd (Gen) and Master of Medicine (Singapore) and pursued her subspecialty training in Breast Surgery. She also completed a 2-year International Fellowship in the field of breast oncoplastic and reconstructive surgery at Siriraj Hospital, Bangkok, Thailand. Apart from being a clinician, Dr Jendana also mentored surgical residents and was a clinical tutor for the Yong Loo Lin School of Medicine at National University Singapore and the Duke-NUS Medical School. She received the “Best Tutor (Surgery) Award” from NUS, “Outstanding Clinical Teacher Award” from the YYL School of Medicine, and the “Special Recognition Award for being a Role Model to the Medicine Graduating Class” from the YYL School of Medicine, NUS.