Blood is normally liquid and exists in our blood vessels, namely our arteries and veins. Its function is to deliver life-giving oxygen and nutrients to all cells in our body via the arteries, and to remove metabolic cellular waste products by way of our veins. Unbeknownst to many, blood also has a solid function – where it turns from liquid to solid a.k.a. blood clot.
An example of normal clot formation is whenever someone sustains a cut injury. Bleeding is caused by the transection of blood vessels, normally the smallest ones called capillaries in flesh wounds, or sometimes, in major arteries/veins in severe injuries. Bleeding may stop when the coagulation cascade within our blood is initiated and liquid blood becomes a clot to plug the cut vessels. However, if clot forms within an otherwise normal blood vessel, it is almost always abnormal.
DEEP VEIN THROMBOSIS (DVT)
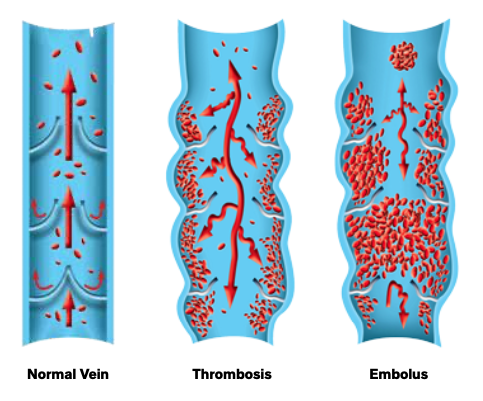
Deep vein clots or deep venous thrombosis (DVT) afflict about 1 in 10,000 people annually. Standard of care treatment is blood thinners or anti-coagulation medications. This is to prevent propagation (growth) of the thrombus (clot) and embolism (breaking off and dissemination into blood stream). If a large DVT from the leg or pelvic veins dislodges and travels to the heart and lungs (called a pulmonary embolus or PE), it can lead to life-threatening heart dysfunction or even death. Hence, the acute phase treatment of DVT in the first 2-3 weeks is to prevent propagation and embolisation.
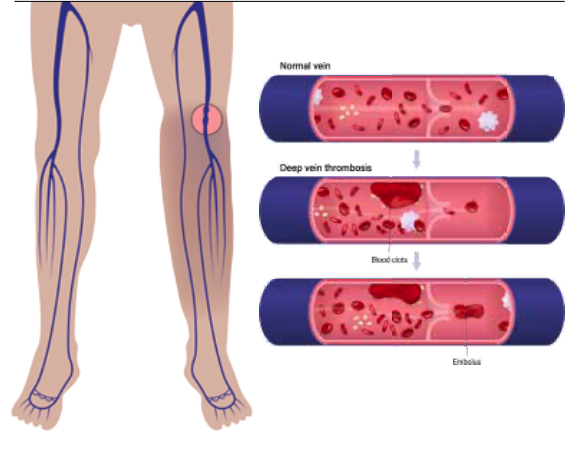
Clot formation in our body is very much like Jell-O (or agar) making. In the beginning when clot forms, it is unstable and friable – just like fresh Jell-O that needs to set with cooling. The early-stage friability contributes to its embolic risk in acute DVT. Subsequently, clots will begin to become organised if our immune system cannot work fast enough to break it down completely. Small clots can resolve completely but large ones may not.
DVT occupies the flow channel within and is therefore obstructive to blood flow, impeding venous return. This can lead to pain, redness and swelling of the affected limb. And with time, just like Jell-O that has been left out for over two weeks, it becomes hard (organised), stuck and impossible to remove. Chronic DVT is known to cause post-thrombotic syndrome (PTS) in up to 40% of patients, who then suffer chronic skin changes (hyperpigmentation, ulcers), varicose veins and persistent limb swelling.
SYMPTOMS

An elderly woman smears a cream or ointment on her leg on a light isolated
Common signs and symptoms of DVT include the following:
- Swelling of affected leg.
- Pain in the leg (calf ) muscles which often starts as achiness, soreness or cramp.
- Red or discoloured skin on the leg.
- Warm feeling in the affected leg.
Do note that DVT may also have no symptoms.
Warning signs and symptoms of PE include:
- Sudden shortness of breath
- Rapid breathing rate (>25 breaths a minute)
- Chest pain that worsens when taking a deep breath or coughing
- Coughing up blood
- Rapid pulse rate (>100 beats/minute)
- Light headedness, feeling dizzy or fainting
If you have any of the above and are concerned about DVT, contact your doctor. And if you develop signs or symptoms of a PE, seek emergency medical help as it is a life threatening complication of DVT.
RISK FACTORS
The main causes of DVT are damage to the vein from trauma, surgery, or inflammation due to infection or injury. DVT has also been observed in COVID-19 patients who are critically ill. Other medical conditions can also alter the “thickness” of blood, such that it is more prone to clotting (hypercoagulable). Some common risk factors include:
- Age: The risk of DVT increases over the age of 60. However, DVT can occur at any age.
- Immobility: Your legs and thighs are very primitive pump systems to help venous blood flow. When your legs are still for hours, your muscles do not contract, and venous blood flow stagnates.
- Injury or Surgery: Direct injury to veins renders them more prone to clotting.
- Birth Control Pills or Hormone Replacement Therapy: These increase the blood’s ability to clot.
- Pregnancy: Pregnancy increases the pressure in the veins in the pelvis, slowing down blood from the lower extremities and making it more prone to clot. This risk continues up to six weeks after pregnancy.
- Overweight or Obesity: This increases the pressure in the veins in the pelvis and legs.
- Smoking: Smoking affects blood clotting and circulation, increasing DVT risk.
- Cancer: Some cancers increase substances in your blood that cause blood to clot. Some forms of cancer treatment also increase the risk of blood clots.
- Heart Failure: This causes overall slowing down of blood circulation, including the venous return. The limited heart and lung function also make symptoms caused by small PEs to be more noticeable.
- Inflammatory Bowel Disease: Conditions like Crohn’s disease or ulcerative colitis increase DVT risk.
- Past/Family History of DVT/PE: Familial links may put one at higher risk.
- Genetics: There are known inherited genetic risk factors or disorders that render clots to form easier, such as factor V Leiden, protein-C and -S deficiency, prothrombin gene mutation 20210, etc.

Sometimes, there are no identifiable risk factors, and this is known as unprovoked DVT.
DIAGNOSIS
The diagnosis of DVT is mainly by duplex ultrasound scan of the lower extremity to visualise the clot within the deep vein. This should be done after thorough evaluation by your doctor. Occasionally, a CT-scan of the abdomen/pelvis is required to visualise DVT that involves the pelvic or abdominal veins. A CT-scan pulmonary angiogram is required to diagnose a PE.
TREATMENT
Treatment of DVT/PE is predominantly medical with blood thinning agents (anticoagulants). Heparin can be given intravenously or by subcutaneous injections, and acts the quickest. As patients are stabilised, blood thinning medications are converted to oral forms so that they can be discharged home. Oral anticoagulants include warfarin and the newer oral anticoagulants (NOAC), such as rivaroxaban or apixaban. Do note that bleeding complications may sometimes occur from anticoagulation treatment of DVT/PE.
More recently, minimally invasive endovascular surgery techniques have become available to “melt” (thrombolysis) the DVT, aspirate (suction thrombectomy), or extract clots away (clot retrieval) to reduce the clot burden in order to prevent long-term complications, such as PTS. Deep venous stenting can be performed in narrowed vein segments such as iliofemoral veins in the pelvis to reduce recurrence of DVT (e.g. May Thurner syndrome). Compression socks have also been shown to be effective in symptom relief and prevention of further complications. These novel treatment approaches are minimally invasive without big cuts, are well tolerated by most patients, and have minimal down time. Hence, they should be offered to the subset of DVT patients who may face life-long debilitating PTS.
LIFESTYLE MANAGEMENT
Some of the things which you can do to prevent DVT include:
- Avoid sitting still. If you are on bedrest (accident or surgery), try and get moving as soon as possible. If you are sitting for prolonged periods, avoid crossing your legs, which can block your venous blood flow. And if you are travelling long distance (plane or car), get up and walk around. If you are traveling by car, stop and take a rest walk every hour. Likewise, walk the aisles hourly if you are in a plane. If you cannot get up to walk, do static exercises, such as heel raises while the toes are on the floor, alternating with toe raises with heels on the floor.
- Exercise and manage your weight. Obesity is a risk factor for DVT. Doing regular exercise lowers your risk of blood clots.
- Stop smoking.
@PRIME