Coronary Artery Disease (CAD) occurs when the major blood vessels that supply the heart become damaged or diseased. This is caused by plaque build-up (cholesterol deposits) along the lining of the arteries, disrupting blood flow to the heart and starving it of oxygen. Before the advent of angioplasty in 1977, CAD was conventionally treated with a Coronary Artery Bypass Graft (CABG). This involves taking healthy blood vessels from the chest, arm or leg to create grafts to bypass the blocked coronary arteries, providing a new path for blood flow around the blocked arteries.
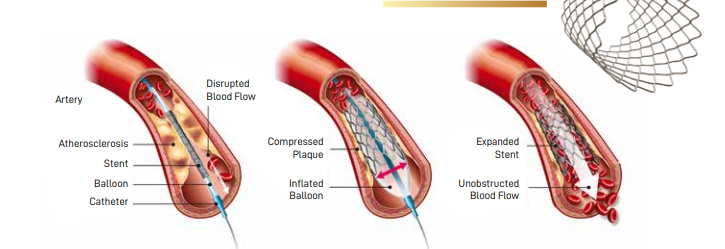
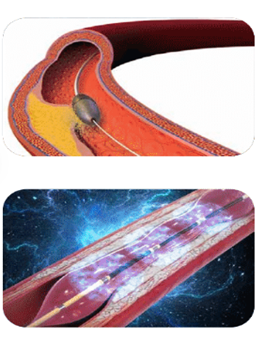
Medical technology advancements brought about a minimally invasive alternative, Percutaneous Coronary Intervention (PCI) or coronary angioplasty. This procedure involves the insertion of a small balloon catheter into the narrowed or blocked vessel to widen the narrowing, improving blood flow to the heart muscles. Often, a heart stent will also be implanted, which helps to prop the vessel open. The stent stays in the vessel permanently to hold it open and improve blood flow. Modern stents are coated with medications that are slowly released to prevent re-narrowing.
With the advancement of PCI technology and techniques, procedures have become relatively safer, yielding better outcomes.
Vascular Access
The contemporary approach for arterial access in PCI over the last decade has been via transradial access (TRA), with the insertion of a small-sized sheath through the radial artery at the wrist using local anaesthesia. This approach reduces bleeding, vascular complications, and improves patient comfort and survival compared to the traditional transfemoral access (TFA) through the groin.
Increasingly, experienced cardiologists are using distal transradial access (d-TRA) through the pulse located at the anatomical snuffbox at the dorsum of the hand. There is emerging evidence that this method provides better patient comfort and, although infrequent, further reduces vascular complications related to TRA.
Coronary Physiology
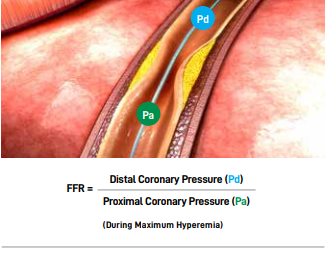
During coronary angiograms, to determine the severity of a narrowing, Fractional Flow Reserve (FFR) can also help objectively determine whether more intermediate forms of narrowing require PCI. This process involves an ultra-thin wire sensor inside the coronary artery that measures the pressure before and after the narrowing. To measure FFR, an ultra-thin wire with a sensor close to its tip is passed into the coronary artery beyond the narrowing. The pressure before and after the narrowing is compared. If there is a significant drop in pressure across the narrowing indicating poor blood flow, PCI will be recommended. If the drop in pressure is modest, medications, rather than PCI, will be recommended. This approach is backed by strong scientific data for the best clinical outcomes.
Coronary Imaging/Intravascular Imaging
Once the decision for PCI or stenting is made, the use of intracoronary imaging can greatly improve the final result of the PCI. Advanced imaging catheters, such as Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT), are used within the coronary arteries to accurately measure the size of the vessel, understand the characteristics of the narrowing and, most importantly, to assist in precise sizing and placement of the stent.
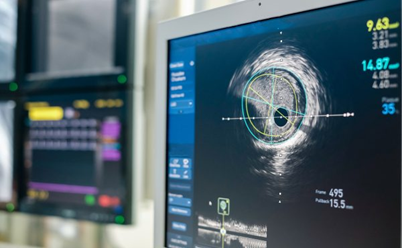
Here is a short explanation of how IVUS and OCT work:
- IntraVascular Ultrasound (IVUS) – Ultrasound waves are transmitted from a miniaturised ultrasound probe on the catheter, which bounces back off the vessel wall, and the information is collected and analysed to form a greyscale image of the coronary artery and its walls.
- Optical Coherence Tomography (OCT) – Near-infrared light is emitted from the catheter, which bounces back off the vessel wall, and the information is collected and analysed to form remarkably clear and detailed images.
Proper interpretation of data by an experienced cardiologist is essential, especially in more complex procedures. Scientific data show that using intracoronary imaging improves stenting results and long-term patient outcomes.
Treating Calcified Vessels
Heavily calcified narrowing is by far one of the toughest conditions to treat. Calcification occurs as part of atherosclerosis (cholesterol plaque build-up) in the coronary arteries and is often seen in the elderly; patients with renal failure; and diabetes patients. A conventional balloon is often inadequate to crack open the rock-hard calcium. Specialised techniques are required, which include:
- Rotational Atherectomy (Rotablation) – This procedure involves a rapidly rotating olive-shaped burr coated with microscopic diamond chips. The burr rotates at very high speeds to drill through the calcified plaque, creating a channel and weakening the hard calcium for balloons and stents to expand.
- Intravascular Lithotripsy (IVL) – This procedure involves using a special balloon catheter with lithotripsy emitters to deliver multiple pulses of sonic waves to fracture the calcified plaque. Once the hard calcium is fractured, the blockage is weakened sufficiently for balloons and stents to expand.
New Generation Coronary Stents
Conventionally, drug-eluting stents (DES) are used in PCI procedures. Made of strong biocompatible alloys, these modern stents are much thinner and more flexible than their predecessors, and are coated with limus-based anti-inflammatory drugs. A substantial amount of clinical data show that the new generation DESs perform exceedingly well, with a good safety profile and very low rates of re-narrowing. Newer innovations in DES include stent platforms which are even more flexible to conform to the natural coronary artery pulsatile movement during each heartbeat.
In selected patients, there is an option of using a bioresorbable scaffold (BRS). BRSs function similarly to DESs and are also coated with anti-inflammatory drugs. However, a BRS is non-permanent and is resorbed over time. Once the scaffold is resorbed, it allows natural vessel pulsatile movement.
Summary
Over the last four decades, advancements in PCI have created new treatment options for patients with CAD. Patients who could only be treated with coronary bypass surgery or medications in the past now have the option of treatment by angioplasty.
From a safer procedure access to newer and more effective stents, we are living in an exciting era where combating coronary artery disease is at the forefront of medical innovation and research. Together with antiplatelet medications and effective cardiovascular risk factor control through medications and lifestyle changes, we can expect to have very good long-term outcomes with PCI.
Dr Joshua Loh
Dr Joshua Loh is a Senior Consultant Interventional Cardiologist and the Medical Director of Capital Heart Centre. He has over 15 years of experience in the field of cardiology, with expertise in the treatment of complex coronary intervention procedures. Dr Loh is experienced in using contemporary technologies to evaluate and manage coronary artery diseases. He is also proficient in providing coronary functional and physiology assessment via flow wire, intracoronary imaging using Optical Coherence. Tomography (OCT) and IntraVascular Ultrasound (IVUS); performing complex coronary interventions such as left main disease, bifurcations, chronic total occlusions, bypass graft interventions and multivessel coronary angioplasty; and treating severely calcified coronary artery disease with specialised devices such as Rotational Atherectomy and Intravascular Lithotripsy.
Senior Consultant Interventional Cardiologist
Capitol Heart Centre
https://capitalhearts.sg
Contact: +6566815677
Whatsapp: +65 88741989
info@capitalheart.sg