Urinary incontinence is any involuntary loss of urine. The risk of developing incontinence increases with age, but younger people may also have it. Women are more likely to suffer from incontinence than men.
Urinary incontinence occurs in 14.5% of people in Asia. It has adverse social, occupational, domestic, physical, sexual and psychological effects on individuals. Although incontinence is a common condition, many people with this condition often delay consulting their doctors and go without treatment. This is because most of them perceive incontinence as part of ageing or they are unaware of available treatments. Some may feel embarrassed discussing their condition with other people.
If you are suffering from incontinence and it is affecting your quality of life, please seek medical advice. In most cases, there will be various treatment options available, including pelvic floor exercises (also known as Kegel exercises), drug treatment or surgery. Your urologist will discuss with you on the best treatment option for you after consultation.
In terms of incontinence, there are basically three different kinds: stress urinary incontinence (SUI), urge incontinence (UUI) and mixed incontinence. We will mainly focus on SUI in this article.
STRESS INCONTINENCE
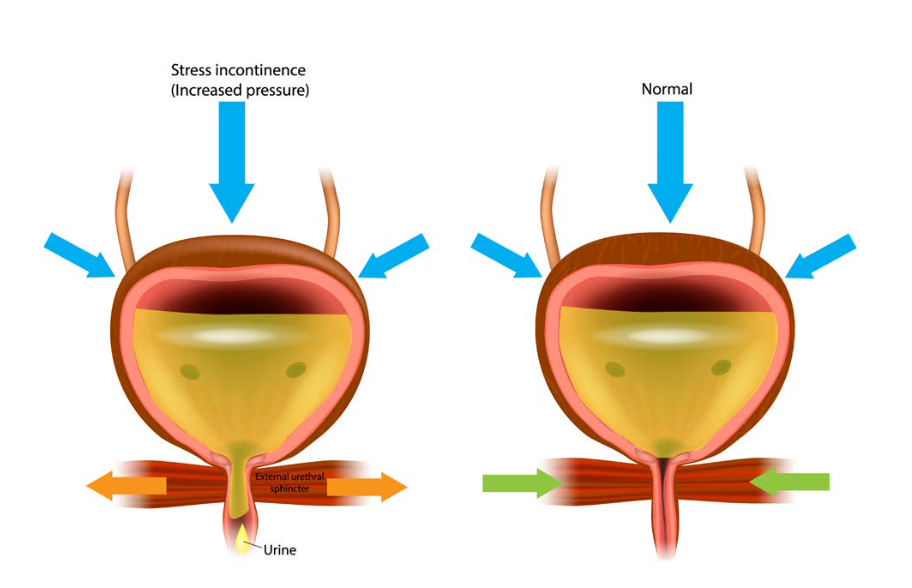
SUI is a condition where you leak urine when there is a sudden increase in pressure on your bladder. This may occur during certain activities like:

- Coughing
- Sneezing
- Laughing
- Exercises like running or jumping
- Lifting heavy things, such as groceries
For people with severe forms of SUI, they may even leak upon sudden movement, such as when moving from a sitting to standing position. When pressure on the bladder increases, the urethra or urinary sphincter simply cannot resist the pressure of a full bladder, and the person leaks urine.
CAUSES OF SUI IN FEMALES
There are a number of possible causes of SUI in females. They include:
- Hormone deficiencies
- Weak pelvic floor muscles
- Menopause and ageing
- Obesity
- Persistent conditions causing cough or constipation
- Childbirth
- Previous pelvic surgery
DIAGNOSIS
Usually, some tests would need to be done for the diagnosis of SUI. Your urologist will take your medical history and do a physical examination. He/she will also need to examine your genitalia area. And where required, other investigative tests may be performed. Let us now take a look at the various diagnosis tools.
MEDICAL HISTORY
Your doctor will take your detailed medical history and ask questions about your symptoms. You may be asked the following questions:
- Description of current symptoms (e.g., number of times you visit the toilet, number of leakages a day, situations when you leak urine, etc.)
- Duration of symptoms
- List of medications you are taking
- Previous surgical procedures
- Other diseases or conditions
- Bowel habits
- Lifestyle (e.g., exercising, smoking, alcohol, diet, etc.)
- Pregnancy history
- Menstruation history and menopausal problems
- Sexual history
PHYSICAL EXAMINATION
For physical examination, your urologist will do a general physical examination on your:
- Abdomen
- Genitals (pelvic examination for females)
GRADING OF SUI
Stress incontinence can be broadly divided into three grades in terms of severity. They are:
GRADE 1 (MILD)
Leakage only occurs when there is severe abdominal straining (e.g., coughing or sneezing). There is generally no need to use pads, and there is no leakage during normal exercise and at night.
GRADE 2 (MODERATE)
Leakage occurs when there is moderate abdominal straining (e.g., running or exercise). There may be a need to use pads and the number of leakages is greater than Grade 1.
GRADE 3 (SEVERE)
Leakage occurs when there is mild stress (e.g., standing up from a sitting or lying down position). There is a need to use pads all the time as the number of leakage episodes is frequent, and this has become a social or hygiene issue.
INVESTIGATIONS
Beyond the aforementioned diagnostic tools, there are other investigative tests that may be done to ascertain SUI. They include:
Urine Test
You will need to give some of your urine for tests to exclude the possible cause of urinary tract infection,which may result in traces of blood in the urine.
Bladder Diary
You may be asked by your doctor to keep a bladder diary. You will note down the amount you drink, how often you urinate, and how much urine you produce. The bladder diary is important because it helps your doctor to understand your symptoms better. You may be asked to buy a measurement jug if you do not have one.
Urodynamic Evaluation (UDS)
A urodynamic test is done to get more information about your urination process, and to check if your bladder muscles/ urinary sphincters work well. During the test, your doctor inserts small catheters in your urethra and rectum to measure the pressure in your bladder and abdomen, while fluid is being instilled into the bladder.
Uroflowmetry
This is a simple test that electronically records the rate of urine flow. It is only done in selected cases and when necessary. You will urinate into a container called a uroflowmeter. This test helps your doctor to check whether there is any obstruction to the flow of urine.
Imaging of the Bladder/Kidneys
This investigation is also only done in selected cases and when necessary. An ultrasound of the bladder and kidneys uses high-frequency sounds to create an image of your bladder/kidneys.
Cystoscopy
This is another test that is only done in selected cases and when necessary. If you have blood in the urine or an abnormal ultrasound finding of the bladder, you may be asked to undergo a flexible cystoscopy in the clinic. This day procedure allows your urologist to look into your bladder to assess if you have any other conditions.
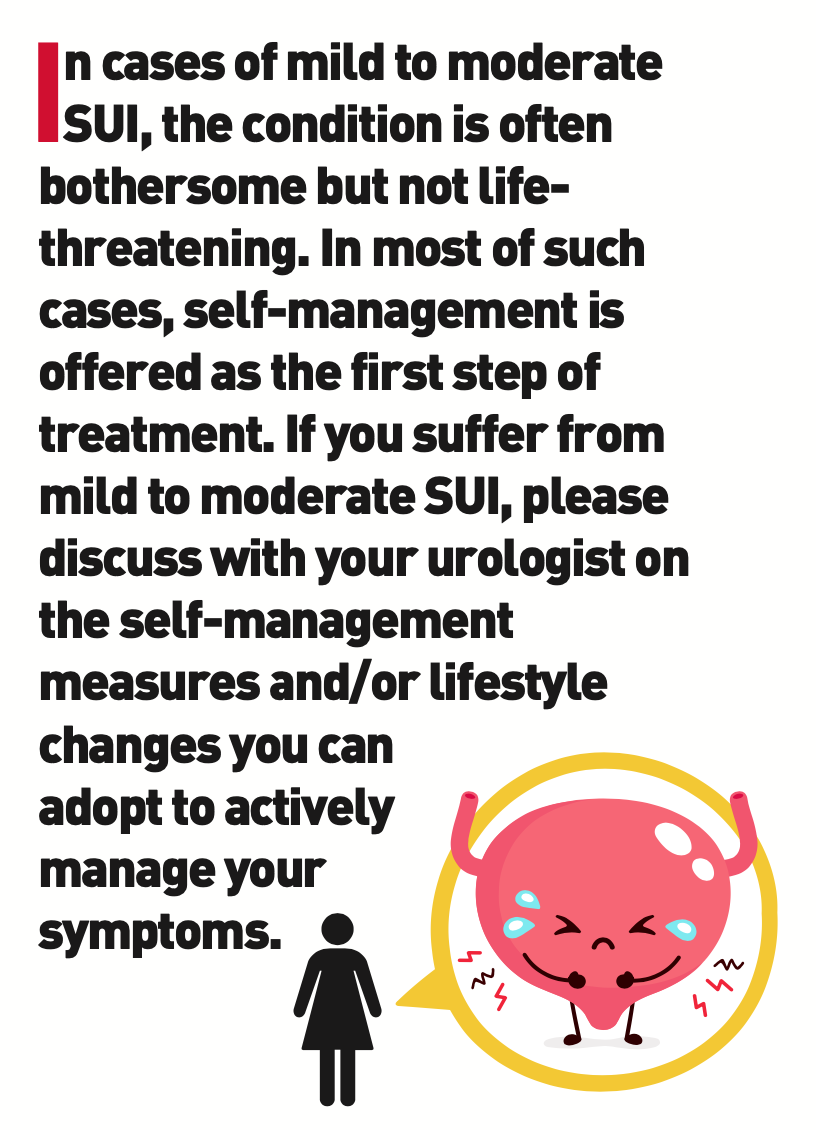
SELF-MANAGEMENT/LIFESTYLE CHANGES
In cases of mild to moderate SUI, the condition is often bothersome but not life-threatening. In most of such cases, self-management is offered as the first step of treatment. If you suffer from mild to moderate SUI, please discuss with your urologist on the self-management measures and/or lifestyle changes you can adopt to actively manage your symptoms. The following self-management measures may be prescribed:

- Fluid restriction
- Use of absorbent pads/adult diapers
- Bladder retraining
- Avoidance of constipation and known triggers
- Weight loss
- Pelvic floor exercises (also known as Kegel exercises)
DRUG TREATMENT
Medications may be required if self-management or lifestyle changes are inadequate to control the symptoms. A common medication is local estrogen application for postmenopausal females to improve their pelvic floor tissues.
SURGICAL TREATMENT
For incontinent patients who desire a better quality of life and/or have failed conservative treatment/Kegels exercise treatment, surgery may be offered. Surgery may involve lifting up the urethra or bulking Up the sphincter muscle SO that the closure mechanism improves. Additional surgeries to correct pelvic organ prolapse may also be necessary.
This is a summary of surgeries that are commonly performed for female SUI.
1. Midurethral Sling (MUS)
This is a strap/ribbon (synthetic mesh) that is placed under the urethra to provide support.
2. Autologous Fascial Sling
This is a strap/ribbon made from the patient’s own body tissue (harvested from the abdomen or thigh) that is placed under the urethra to provide support.
3. Burch Colposuspension
This is an operation to support the bladder neck, which connects the bladder to the urethra to resist pressure.
4. Artificial Urinary Sphincter (AUS)
An inflatable cuff placed around the urethra connected to a hand-controlled pump that allows you to pass urine when released. For patients with mild/grade 1 SUI, other newer, minimally invasive experimental methods may be used. These include:
1. Transurethral Injection of Bulking Agents
In this minimally invasive procedure done under local anaesthesia or sedation, a biocompatible substance, such as collagen, is injected into the urinary sphincter region to improve the closure mechanism to prevent leakages. The short-term success rate of this procedure is around 60-70% for symptom improvement. A repeated injection may be required if there is symptom recurrence or inadequate improvement.

2. FOTONA Laser
The FOTONA laser is a technology that utilises thermal energy to affect the vaginal tissues. Collagen remodeling is stimulated and new collagen fibres are synthesised. The vaginal mucosa (inner lining of the vagina) and collagen-rich endopelvic fascia (connective tissue enveloping pelvic organs) shrinks and tightens, providing greater support to the bladder. This allows for the return of normal continence function.
This procedure is non-invasive and ensures quick recovery without the need for analgesics or antibiotics. Two to three sessions are required at monthly intervals. Repeated sessions may be needed.

3. Electromagnetic Stimulation (HIFEM)
In this procedure, the patient sits on a chair/device that uses HIFEM to stimulate the pelvic floor muscles. A HIFEM session triggers intense pelvic floor muscle contractions by targeting neuromuscular tissues and inducing electric currents. This directly modifies the muscle structure, bringing about more efficient growth of muscle fibres and the creation of new protein strands. Incontinent patients who were once unable to perform high-repetition pattern exercises due to pelvic floor muscle weakness can restore neuromuscular control after HIFEM treatment.
This treatment is especially useful for individuals who are unable to isolate their pelvic floor muscles during Kegels, or for patients who are not keen or suitable for more invasive treatments. PRIME
Dr Fiona Wu
Medical Director and Consultant Urologist, Aare Urocare
MBBS (S’pore), MRCS (Edin), MMED (Surg),
FRCS (Urol) (RCPSG), FAMS (Urology)
Dr Fiona Wu graduated with the degrees of Bachelor of Medicine and Bachelor of Surgery from the National University of Singapore (NUS). She obtained a surgical fellowship with the Royal College of Surgeons in Edinburgh in 2008. Prior to ther private practice, Dr Wu spent 15 years in public service. She was a Consultant in the Department of Urology at NUH, Alexandra Hospital and NTFGH. Dr Wu has special interests in the field of Female Urology, Neuro-Urology and Reconstructive Urology. Her clinical interests include treating incontinence in a holistic way using minimally invasive methods. She worked closely with the hospital gynaecology and colorectal departments to treat complex pelvic floor conditions and continues to do so in her own practice.